There have been lots of stories about new cancer treatments recently, including a personalised vaccine, a vaccine for skin cancer, and new drugs for lung and bowel cancers. These treatments have been called a “game-changer”, and “extremely impressive”, with results “off the charts”. We sat down with one of our senior scientists, Sarah Kefyalew (pictured), to find out more.
There have been lots of stories about new cancer treatments recently, including a personalised vaccine, a vaccine for skin cancer, and new drugs for lung and bowel cancers. These treatments have been called a “game-changer”, and “extremely impressive”, with results “off the charts”. We sat down with one of our senior scientists, Sarah Kefyalew (pictured), to find out more.
With all the exciting treatments coming out, does this mean we’re getting closer to finding a cure for cancer?
The recent news around drugs and vaccines, many of which were presented at a recent conference in America, show the great advancements in cancer therapeutics.
It’s important to note that cancer is not one disease, but many different types. These new drugs and vaccines each target one cancer type and, combined with chemotherapy and surgery, have shown great improvements in cancer survival rates.
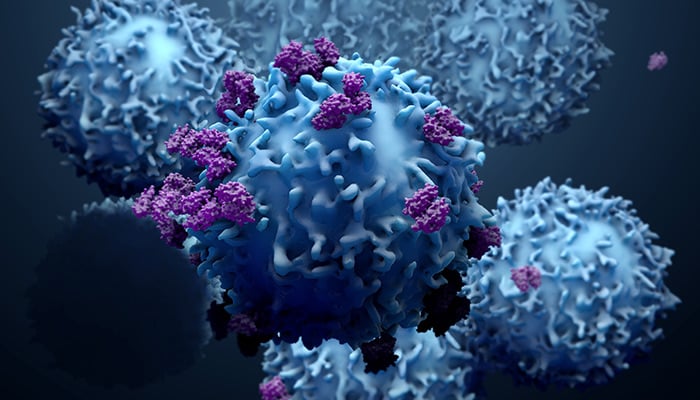
Most of the cancer vaccine trials look at the effects of the vaccine in combination with immunotherapy. While we don’t know the effects of the vaccine on its own, these findings add to our arsenal of treatments for cancer. These drugs and vaccines either increase the likelihood that immunotherapy will treat the tumour or allow the tumour to be removed with surgery. Additionally, some of these drugs don’t treat the tumour itself but reduce the risk of it progressing and spreading to other parts of the body.
If these trials are showing good results, will the new drugs and vaccines be widely available soon?
These drugs and vaccines are still in their trial stage. If the trials continue to show positive results, the researchers hope that the drugs may be available to the wider population in a few years.
They still need to be tested in more people – for example, a study investigating the effects of a drug for bowel cancer was only conducted in 32 patients. We also need to see how effective these treatments are in improving long-term survival rates.
Once they are shown to be effective, they still need to be approved for use. One of the drugs making the news recently is Enhertu, which has been approved for use in Scotland, but not in England and Wales.
Will these new drugs work for everyone?
Cancer treatments are getting increasingly personalised, and these new drugs only work on those whose cancers display a specific genetic profile. For example, 15% of those with stage 2 or 3 bowel cancer have the genetic make-up that could allow them to be treated with the new drug being trialled (pembrolizumab).
Even if someone is considered suitable to be treated with one of these drugs or vaccines (for example if they have the specific genetic profile), it doesn’t guarantee the cancer will be cured. Though these treatments are very promising, they don’t have a 100% success rate, so other treatments may be required.
World Cancer Research Fund looks at how what we eat, and how active we are, affect quality of life during cancer, and the chances of cancer coming back. If we have all these new treatments, why do we need more research into causes?
Hopefully, these new treatments will lead to increases in survival rates, and more people living longer after a cancer diagnosis. However, it’s much better to prevent cancer in the first place, and we should not be complacent in our cancer prevention efforts.
These therapeutics are at various stages of development and may not work for everyone. While this news is promising, it’s important, as much as we can, to follow our Cancer Prevention Recommendations.
Cancer, even when there are effective treatments, can have really debilitating side-effects, as can many of the treatments. Even once treated, it can impact quality of life in a variety of ways, such as fatigue, and increasing the risk of other diseases after a diagnosis.
This is why we fund research to understand the associations between risk factors which increase the likelihood of cancer, and how these may impact quality of life after a cancer diagnosis.