It has long been established that junk food advertising drives consumption of unhealthy food and drink, shaping preferences from a young age and contributing to overweight and obesity.
The strength of the evidence base is perhaps best corroborated by the enormous advertising budgets of unhealthy food and drink companies. If advertising didn’t pay off, why would Coca-Cola allocate a whopping $5 billion to their worldwide advertising budget in 2024?
Restricting junk food advertising is therefore a powerful and proven public health measure. Yet, most recently, you may have seen measured responses from public health advocates in the UK, including World Cancer Research Fund, upon the introduction of long-awaited junk food advertising restrictions in January 2026.
Marketing regulations can underdeliver
The bottom line is that whilst the UK’s restrictions mark a step forward in protecting children’s health at a time when obesity rates continue to rise, they have been weakened and delayed by industry influence – most notably through the introduction of a sweeping brand exemption. This significantly undermines the policy in two key ways. First, it allows brands that are synonymous with foods high in fat, salt and sugar (HFSS) to continue being advertised – think the famous Golden Arches. Second, the lack of brand restrictions enables companies to promote entire HFSS product ranges, just not individual products. Ultimately this preserves brand visibility and influence while circumventing the spirit of the regulations.
The brand exemption is not the only weakness of the advertising restrictions. Work on this policy began as far back as 2018, and in the years since, the marketing landscape has evolved dramatically. Simply put, the regulations are not a match for the rapidly changing marketing landscape. For example, direct marketing channels, such as email and text messaging, remain unchecked, allowing unhealthy food and drink companies to continue targeting consumers.
The unseen cost of delays and dilution
The unfortunate tale of industry influence is not unique to the UK. Globally, efforts to curb the scourge of junk food on society are denied, diluted, derailed and delayed by industry.
Marketing restrictions are difficult to get over the line. In the UK, the policy was subject to five separate consultations and four delays to its rollout. That is an immense amount of government time, effort and resources. Moreover, the burden it places on the public health sector, which often operate under capacity constraints, must be acknowledged.
We also need to recognise that obesity, a key risk factor for cancer, is linked to deprivation. In many countries, those living in the most deprived areas are more likely to be living with obesity compared to those in the most affluent communities. Delays or failures to implement effective policies therefore disproportionately impact those who are already most vulnerable.
Industry opposition at full throttle
The resistance we see to advertising restrictions can partly be explained by the fact that marketing is not a peripheral commercial function. Instead, it sits at the very core of food and drink businesses, playing a pivotal role in building brand value, customer loyalty and long-term profitability.
Marketing restrictions are also unusually visible. Unlike reformulation targets or nutrient thresholds, which operate largely behind the scenes, advertising bans are immediately noticeable. They can also be drawn into wider debates around personal responsibility, censorship and creativity – making the more contested and politically charged. They tend to hit a nerve.
Recognition of these issues is not a justification for inaction. The reality is that companies by their very nature are required to innovate, and they can do so in a way that supports public health rather than undermining it.
Action must go beyond the status quo
Let’s be clear, no one is suggesting that junk food marketing restrictions alone will solve the obesity crisis. However, the version we’ve seen introduced in the UK will most certainly underdeliver, especially given the restrictions don’t sit within a broader framework of measures designed to improve the nation’s diet yet. Countries in Latin America, including Chile and Mexico, have taken more holistic approaches which embed marketing restrictions within a wider set of measures including mandatory warning labels and robust school food standards
But when governments introduce policies that appear ambitious on paper but lack the strength to deliver in practice, they risk entrenching the status quo while giving the impression of action. This pattern is not unique to food. Similar delays and dilutions are seen across alcohol, gambling and other health-harming industries, where commercial interests routinely take priority over public health.
Ultimately, the question is not what needs to be done, but what governments are willing to do to protect public health.
With the UK Labour Party in government for just over a year, this year’s Party conference provided a valuable opportunity to take stock of the progress made on health and identify areas in need of improvement.
Academics, people with lived experience, and experts from thinktanks and charities congregated in Liverpool in September to share how the government can be bolder on prevention – here are my top five takeaways:
1) Tackle poverty alongside prevention
Just before conference, the government published its 10 Year Health Plan for England, setting out a raft of policy priorities to achieve its health mission. Positively, a key theme throughout the Plan was the need to tackle health inequalities – the systematic and unfair differences in health between different groups of people – especially through prevention.
At an IPPR and Impact on Urban Health fringe event, “Can the Government deliver its long-term health mission?”, speakers made impassioned pleas about the need to address the social determinants of health. Dr Sonia Adesara, a practising GP and Vice Chair of the Fabian Society, explained that while she may be able to treat the symptoms and health issues that manifest as a result of living in poverty, such efforts are in vain if the government does not tackle the root causes of ill health.
These drivers are wide ranging, from poor food environments, where junk food is the cheapest and most available option, to substandard housing. Crucially, addressing them requires the adoption of a truly cross-governmental approach. As Peter Babudu, the Executive Director at Impact on Urban Health, put it, even the Department for Health and Social Care at its very best cannot tackle these complex issues alone.
These are subjects World Cancer Research Fund has engaged with significantly through our blog series on health inequality and cancer.
2) Prioritise public health over industry interests
Another hot topic at conference was the need to place public health above vested interest. The history of industry derailing, delaying and diluting public health policy in pursuit of profit has long been documented both in the UK and abroad. Yet, the food and drink industry continues to play a key role in various policy development processes under Labour.
The delayed junk food marketing ban provides a clear example of why the government needs to make a concerted effort to tackle vested interests. October was meant to see the implementation of a key manifesto pledge: a watershed ban on junk food advertisements. Instead, the ban, which could have a profound effect on reducing childhood obesity, has been delayed yet again. Worse, industry lobbying has resulted in a complete brand exemption. In practice, this means that products like Cadbury Diary Milk, Mars bars, and Coca-Cola can still be advertised because they are not only products but brands as well.
Walking through the exhibition hall, the presence of industry was hard to miss, with prominent stands for Heineken and Sainsbury’s – a reminder that just like those of us in public health, industry is also working hard to influence government.
3) Bring the public along on prevention
Action to improve public health is often depicted, especially in the media, as “nanny-statism”. At Nesta’s event, “How can the government make its health reforms a success?”, Kevin McKenna, the MP for Sittingbourne and Sheppey and a former NHS strategist, insisted that we need to communicate more clearly with the public about why the 3 health shifts (sickness to prevention, analogue to digital, and hospital to community) are so important. Ultimately, we need a more compelling case to counter the “nanny-state” narrative, which does not reflect the public’s views. Polling consistently shows strong support for government action to improve health and reduce inequalities.
Meanwhile, at Demos’ fringe “Prevention: From overlooked to mission critical”, Prof Gurch Randhawa, Director of the Institute for Health Research, emphasised the importance of approaching prevention in a culturally sensitive manner so that everyone benefits. For example, schemes providing healthy food to those in need must take into consideration the food preferences and dietary requirements of the diverse communities they serve.
The task of bringing the public along on the prevention agenda does not rely solely on the government – charities, including ourselves, can play an important role. Our brilliant Health Information team’s work educating the public on how they can reduce their risk of developing cancer through good nutrition and an active lifestyle is just one example.
4) Beware the temptation of silver bullets
Despite the recognition of the need for a health-in-all-policies approach, the temptation of “silver bullets” and quick fixes loomed. This was particularly notable in discussions around weight-loss jabs.
In the UK, obesity is the second biggest cause of cancer after smoking. Addressing this crisis requires a coordinated approach that includes both prevention and equitable access to treatment. However, in his conference speech, the Health Secretary, Wes Streeting, didn’t quite echo these sentiments. Instead, he declared that “weight-loss jabs could help us finally defeat obesity”, while failing to mention the need to fix our broken food environment.
The hype around weight-loss drugs was reflected in long queues for a New Statesman event hosted in partnership with Eli Lily, a pharmaceutical company that produces appetite suppressants.
Wearable tech also came up in a similar context, with suggestions that it could revolutionise how individuals take charge of their own health. It was positive that the need for digital inclusion was recognised, but again, we need to ensure that proven policy interventions, such as salt and sugar taxes, remain the first port of call.
5) Reducing alcohol harm is key
One glaring omission was the absence of discussion on alcohol harm, especially given that alcohol deaths have reached record highs across the UK.
Charities including the Forward Trust ensured the issue was still on the agenda, hosting a sober reception as part of their work to advocate for alcohol-free spaces at conference.
We also highlighted alcohol harm, building on this summer’s Cancer Prevention Action Week, which sparked a national discussion on the link between alcohol and cancer. This included meeting with Dr Scott Arthur MP at conference to discuss alcohol-related cancer and the urgent need for government to deliver on its commitment to introduce mandatory alcohol labelling, ensuring that labels make the cancer risk of alcohol explicit.
The prevention mission is here to stay
Despite the long way we have to go, one thing is abundantly clear: the prevention mission is here to stay.
Fortunately, there are several critical influencing opportunities on the horizon where the government can apply these lessons from conference, such as the forthcoming National Food Strategy. Over the coming months, we’ll be working hard to hold the government to account in delivering on cancer prevention and survivorship.
If you’d like to keep up to date with our work, sign up to our monthly Policy and Public Affairs newsletter. If you have any thoughts on what we’ve covered in this blog, we’d love to hear from you! Get in touch with us at policy@wcrf.org.
The UK government published its 10-year Health Plan on 3 July, setting out its ambitions to reform the health system and shift the focus from sickness to prevention.
As a cancer prevention charity with a vision of a world where no one dies from a preventable cancer, we welcome the Plan’s direction but there are many key areas of health policy where it simply falls short of what the public needs.
Positive inclusions
Many of the commitments in the Plan had already been announced and were warmly received, such as the expansions of free school meals and the Soft Drinks Industry Levy.
Encouragingly, the Plan also includes new mandatory measures that mark a meaningful step towards creating healthier environments for all.
These include:
- Mandatory healthy food sales reporting for all large companies in the food sector.
- Mandatory healthy food standard to improve the healthiness of sales.
- Updates to the nutrient profile model, used to set marketing restrictions on junk food.
- 10% uplift to restore the value of the Healthy Start scheme from 2026–27.
- Mandatory labelling on alcoholic drinks to include consistent nutritional information and health warning messages.
- Place-based approach to physical activity, including £250m for 100 places via Sport England, at least £400m for local community sports facilities, and new school sport partnerships.
- National walking and running campaign led by Sir Brendan Foster.
- Development of a new physical activity strategy.
These measures are welcome steps forward in improving our food and drink environment and enabling people to be more physically active.
We hope the forthcoming National Food Strategy will drive deeper systemic changes to ensure affordable, accessible healthy food for everyone in England.
Critical missed opportunities
On alcohol, the Plan falls short of prioritising the range of evidence-based policies proven to reduce alcohol consumption, which causes around 17,000 UK cancer diagnoses each year.
Notably, it fails to include minimum unit pricing (MUP) for alcohol in England, despite the success of MUP in reducing alcohol-related deaths in Scotland and Wales. Worryingly, England continues to lag the devolved nations on this crucial policy.
The Plan also makes no mention of strengthening marketing restrictions on alcohol, and so enables industry to continue to normalise drinking as an aspirational lifestyle choice.
Given the rising number of alcohol-related deaths each year, we are urging the UK government to deliver a National Alcohol Strategy for England. As outlined in our recent letter to the Prime Minister, Keir Starmer, during Cancer Prevention Action Week, we continue to call for bold action on alcohol-related cancer.
Equally disappointing is the absence of action to strengthen protections and support for breastfeeding and infant feeding. There are no new mandatory, independently enforced regulations on the composition, marketing and labelling of baby and toddler foods. This is a missed opportunity, particularly in light of the UK government’s stated goal to raise the healthiest generation of children ever.
We will continue to urge the government to adopt the recommendations of the Competition and Markets Authority’s market study on infant and follow-on formula.
Turning ambitions into action
This Plan arrives as Labour marks its first year in government under Starmer. This government now has the opportunity – and responsibility – to turn its prevention agenda into lasting structural change that improves the nation’s health.
The upcoming National Cancer Plan for England presents a further chance to address modifiable risk factors and fill the gaps left by the 10-year Health Plan.
We welcome the Prime Minister’s willingness to challenge accusations of “nanny statism” and urge the government to ensure all health strategies are protected from undue industry influence.
We want prevention to be the foundation of all health strategies. We stand ready to bring our scientific and policy expertise to the table – and we’re calling on the UK government to work with us to turn bold ambition into real change, helping millions live longer, cancer-free lives.
In our resource library
Further reading
As part of Cancer Prevention Action Week 2025, on Wednesday we handed in an open letter and petition, alongside breast cancer survivors Dr Liz O’Riordan and Nikki Bednall, and the Alcohol Health Alliance.
The letter (below) – signed by more than 25 organisations and health experts – and the petition called on Prime Minister Sir Keir Starmer and his government to introduce a National Alcohol Strategy to Prevent Cancer, as part of our Cancer Prevention Action Week (CPAW) activity.
This year, CPAW is highlighting the links between alcohol and cancer – our research shows that most people don’t know that drinking any amount of alcohol increases the risk of 7 types of cancer.
What’s more, around 17,000 new cases every year are down to alcohol – so we’re urging the UK government to introduce a long-overdue National Alcohol Strategy for England – one that tackles alcohol harm head-on through:
- mandatory health warnings highlighting cancer risk
- minimum unit pricing
- marketing restrictions
to reduce consumption, lower cancer risk, and protect lives.





Read the full letter below
The Rt Hon Keir Starmer MP
Prime Minister
10 Downing Street
London SW1A 2AA
CC: The Rt Hon Wes Streeting MP, Secretary of State for Health and Social Care
Ashley Dalton MP, Parliamentary Under-Secretary of State for Public Health and Prevention
25 June 2025
The UK government must act on alcohol now to prevent cancer
Dear Prime Minister,
On behalf of more than 20 organisations and public health leaders, we are writing to share our deep concern about the continued lack of action to reduce alcohol consumption across the United Kingdom. In particular, the absence of a National Alcohol Strategy for England stands in stark contrast to the scale of harm caused by alcohol, with alcohol-specific deaths having increased by 42% in England between 2019 and 2023 alone.
This week marks Cancer Prevention Action Week (CPAW) – a national campaign led by World Cancer Research Fund (WCRF) – which seeks to empower the public and inspire change to prevent cancer. This year, CPAW is shining a spotlight on the link between alcohol and cancer, and the urgent need for government action.
In the UK, alcohol causes around 17,000 cases of cancer every year – equivalent to 46 people receiving a diagnosis every single day. And as our population ages and grows, these numbers are projected to rise. Worryingly, the pandemic has also driven an increase in high-risk drinking. Modelling by the Institute of Alcohol Studies and Health Lumen suggests that if this trend persists, we could see an additional 18,785 cancer cases by 2035.
Public awareness remains alarmingly low that alcohol is a Group 1 carcinogen, the same category as tobacco and asbestos, and a cause of seven types of cancer, including two of the most common breast and bowel as well as mouth and throat, oesophageal, liver and stomach cancer. These risks are present even at low levels of consumption. New polling commissioned by WCRF reveals that when asked unprompted only 1 in 14 UK adults are aware that alcohol increases cancer risk and 25% believe there is no health risk attached to drinking alcohol.
We are not alone in our concern – thousands of members of the public including more than 20 organisations have signed our petition calling for greater government action. They agree that no one should have to suffer the devastating trauma of alcohol-related cancer.
The human toll is compounded by the economic burden. In 2016, Cancer Research UK estimated that alcohol-attributed cancers cost the NHS alone an estimated £100 million annually. With the health service under immense strain, it is imperative to act now and realise the government’s priority of prevention.
Despite alcohol being the sixth leading cause of preventable cancer in the UK, current policy does not reflect this reality. We urge the government to fulfil its responsibility to protect public health by introducing a National Alcohol Strategy for England without delay, which must include:
- Mandatory alcohol product labelling with health warnings, including information on cancer risks and calorie content.
- Marketing restrictions on alcohol by classifying it as an ‘unhealthy product’ under high fat, salt and sugar marketing restrictions.
- Implementing and evaluating minimum unit pricing at 65p in England with rates adjusted in line with inflation, to bring England into line with Scotland, Wales and Northern Ireland who all either have MUP already or have stated their intention to implement.
It is vital that this strategy aligns with the forthcoming National Cancer Plan for England, ensuring that alcohol is comprehensively addressed as a modifiable risk factor for cancer. We also urge the UK government to work in close collaboration with the devolved administrations, particularly to enable action to improve approaches to labelling and advertising. All policy development processes must be protected from industry influence and vested interests to ensure public health is placed above profit.
Such action would not only help to reduce cancer risks but reduce other alcohol-related harms. It would also support the government’s own ambitions to shift from sickness to prevention, as set out in the Health Mission, and contribute to economic growth by reducing illness-related inactivity.
We stand ready to support this effort and urge you to act now. Together we can tackle the devastating impact of both alcohol harm and cancer.
Yours sincerely,
Rachael Gormley, Chief Executive, World Cancer Research Fund
Dr Richard Piper, CEO, Alcohol Change UK
Alison Douglas, Chief Executive, Alcohol Focus Scotland
Professor Sir Ian Gilmore, Chair, Alcohol Health Alliance
Greg Fell, President, Association of Directors of Public Health
Dr Heather Grimbaldeston, Chair, BMA Public Health Medicine Committee, British Medical Association
Professor David Strain, Chair, BMA Board of Science, British Medical Association
Thalie Martini, Chief Executive Officer, Breast Cancer UK
Eddie Crouch, Chair, British Dental Association
Pamela Healy OBE, Chief Executive, British Liver Trust
Jill Clark, Chair, CancerWatch
Alison Wise, Communications Manager, on behalf of Fight Bladder Cancer
Ailsa Rutter OBE, Director, Fresh and Balance
Kostas Tsilidis, Associate Professor of Cancer Epidemiology and Prevention, Imperial College London
Dr Katherine Severi, Chief Executive, Institute of Alcohol Studies
Dr Dominique Florin, Medical Director, Medical Council on Alcohol
Daniela Binnington Nessman, Founder, Menopause and Cancer
Gopika Chandratheva, Nutritionist, NHS
Tamara Khan, CEO, Oracle Head & Neck Cancer UK
Jon Coleman-Reed, Head of Operations, Prevent Breast Cancer
Dr Claire Shannon, President, Royal College of Anaesthetists
Robert Steele, Chair, Board Directors, Scottish Cancer Foundation
Dr Alastair MacGilchrist, Chair, Scottish Health Action on Alcohol Problems
Chris Curtis, Chief Executive Officer, Swallows Head & Neck Cancer Support Charity
Amandine Garde, Professor of Law & Non-Communicable Diseases Research Unit, University of Liverpool
Richard Cooke, Professor of Health Psychology, University of Staffordshire
Dr Kathryn Scott, Chief Executive, Yorkshire Cancer Research
Only 16% of us in the UK feel at ease discussing our relationship with alcohol, ranking it among the least talked about topics – less so than sex (17%) and money (29%), according to our poll.
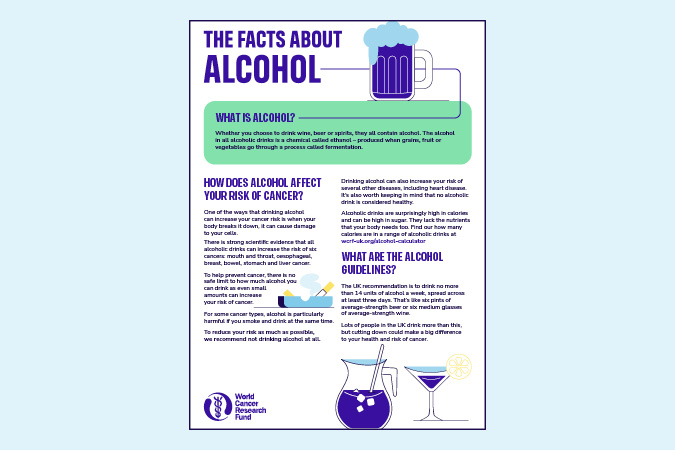
We’re emphasising the connection between alcohol and cancer as part of Cancer Prevention Action Week, which starts today. We have strong evidence that alcohol increases the risk of 7 cancers:
- Breast
- Bowel
- Head and neck
- Oesophageal
- Liver
- Stomach
Alcoholic drinks are also high in calories and often high in sugar, increasing the risk of gaining weight. Living with overweight or obesity increases the risk of at least 13 types of cancer.
We surveyed 2,000 people to gain insights into Britain’s understanding of alcohol and cancer risks. The findings reveal consistent misconceptions regarding alcohol’s dangers. Alarmingly, 25% of respondents did not associate any health risks with alcohol, and only 1 in 14 mentioned cancers as a risk when asked unprompted.
These misconceptions may hinder our ability to have informed conversations about alcohol. About 4% of cancer cases in the UK are attributed to alcohol, meaning that, each year, around 17,000 people are diagnosed with cancer caused by alcohol. Adding to this immeasurable human cost is the economic burden. Alcohol-related cancers cost the NHS around £100m every year.
We need a National Alcohol Strategy
We support clearer public health messaging to raise awareness of the real dangers of alcohol consumption, as well as other measures such as health warning labels. Alongside many other health organisations in the UK, we’re urging the Prime Minister, Sir Keir Starmer, to implement a National Alcohol Strategy for England.
World Cancer Research Fund CEO Rachael Gormley
Alcohol is pervasive in our lives, from celebrations to after-work drinks. But do we truly understand the risks involved? It’s essential that we engage in more discussions about alcohol and cancer, empowering individuals to make informed health choices.
Alcohol Health Alliance Chair Sir Ian Gilmore
One of the reasons public awareness is so low is that we're being kept in the dark about the true cost of drinking. People have the right to know the full picture so that they can make informed choices about what they consume.
World Cancer Research Fund Executive Director of Research and Policy Dr Giota Mitrou
A long-overdue National Alcohol Strategy in England would help the government tackle alcohol harm head on – reducing consumption, lowering cancer risk, and protecting lives.
Nikki Bednall is a World Cancer Research Fund Supporter and breast cancer survivor. She said: “I always thought drinking a few times a week was fine. I never knew it could raise my cancer risk. If I’d known earlier, I might have made different choices. Though hindsight is easy, my perspective has changed with the knowledge that came after my diagnosis.”
Drinking habits in the UK paint a concerning picture in comparison with other nations. Organisation for Economic Cooperation and Development (OECD) 2021 data showed that alcohol consumption in the UK was 10 litres per capita – 16% more than the OECD average of 8.6 litres.
Covid led to an increase in the number of high-risk drinks, with the heaviest drinkers increasing their consumption the most. These changes have persisted beyond the national lockdowns of 2020 and 2021, and subsequently there has been a year-on-year rise in alcohol-specific deaths, which reached an all-time high of 10,473 in 2023.
The research was conducted by Opinion Matters, among a sample of 2,000 nationally representative UK adults. The data was collected between 21.03.2025–24.03.2025.
Cancer Prevention Action Week (CPAW)
This year we’re highlighting the links between alcohol and cancer.
Alcohol and cancer: let’s talk – that was the theme of this year’s Cancer Prevention Action Week. For 7 days on 23–29 June, we talked to politicians, gave radio interviews and spoke to experts about alcohol and cancer. Plus, we shared news and views across our socials:
Facebook | LinkedIn | Instagram | Bluesky
How Cancer Prevention Action Week unfolded
Monday’s highlights
> Brits find it harder to talk about alcohol than sex or money
Yorkshire GP speaks out in support of CPAW:
Dr Nigel Wells, Medical Director and Executive Director Clinical & Care Professional Humber and North Yorkshire ICB and practising GP:
As a GP, I know people can be reluctant to talk about alcohol or share concerns about their drinking – so it doesn’t surprise me that only 2 in 10 people across Yorkshire and the Humber feel comfortable doing so.
But alcohol isn’t harmless – it increases the risk of 7 types of cancer, and, too often, people simply aren’t aware. If this campaign helps someone pause and ask whether alcohol might be affecting their health, and encourages them to speak to a healthcare professional, it will have made a real difference. We need to make these conversations as routine as those about smoking or diet – and that starts with creating a safe, non-judgemental space in every consultation.
We tabled an Early Day Motion in support of Cancer Prevention Action Week. And Alcohol Focus Scotland, a key supporter of this year’s campaign, tabled a motion in the Scottish Parliament on alcohol and cancer.
Tuesday’s highlights

Alcohol Focus Scotland organised a photo call at Holyrood with Members of the Scottish Parliament (MSPs). Photographed are 11 MSPs, including the Cabinet Secretary for Health Neil Gray; Jackie Baillie, Labour’s deputy leader and health spokesperson, and Presiding officer Alison Johnstone. Read more on LinkedIn
Sheridan Dixon, of South Tyneside, was interviewed on ITV Tyne Tees about how she has reduced her drinking as part of efforts to stay cancer free. We’re grateful to our partner Balance North East for helping us share Sheridan’s story.
Wednesday’s highlights

We headed to No 10 Downing St to present our petition to UK Prime Minister Sir Keir Starmer.
Prof Lord John Krebs, Chair of our Global Cancer Update Programme, tabled questions in the Lords on the links between alcohol and cancer, keeping the issue high on the political agenda:
Lord Krebs’ questions to the Lords
-
1
Lord Krebs to ask His Majesty’s Government what steps they are taking to reduce alcohol consumption as a modifiable risk factor for cancer.
-
2
Lord Krebs to ask His Majesty’s Government whether the national cancer plan for England will address alcohol consumption as a modifiable risk factor for cancer.
-
3
Lord Krebs to ask His Majesty’s Government what assessment they have made of public awareness levels of the link between alcohol consumption and cancer risk.
-
4
Lord Krebs to ask His Majesty’s Government what consideration they have given to classifying alcohol as an unhealthy product under high fat, sugar and salt marketing restrictions to (1) strengthen limits on alcohol advertising, and (2) reduce alcohol exposure among vulnerable populations, including children and adolescents.
-
5
Lord Krebs to ask His Majesty’s Government what assessment they have made of the impact of minimum unit pricing on alcohol-related cancer incidence.
CPAW supporter Prof Richard Cooke published research showing that policymakers and drinkers are speaking different languages when it comes to alcohol consumption. He says: “Policymakers need to construct policies to reflect the importance of emotions in drinkers’ narratives. This fits in with psychological theories of drinking behaviour which propose that people drink for different reasons.”
> The language of alcohol: Similarities and differences in how drinkers and policymakers frame alcohol consumption, published in Drug and Alcohol Review
Thursday’s highlights
Health professionals can be instrumental in helping individuals reset their relationship with alcohol and we supported them with a free webinar on Alcohol and cancer risk: What every health professional needs to know.
In the This Is Powerful podcast, Paul Sculfor talked to nutrition expert Dr Federica Amati about alcohol and cancer.
Friday’s highlights
On the blog: It’s mocktail Friday! Start your weekend early with some fizzy fruity creations
Saturday and Sunday’s highlights
Time to take a breath … alcohol is a major part of how many of us socialise, relax and celebrate. But nearly 4% of cancer cases in the UK are down to alcohol – around 17,000 new cases every year.
We hope this Cancer Prevention Action Week has given you an insight into the risks we’re all taking when we drink.
Our research shows that most people don’t know that drinking any amount of alcohol increases the risk of 7 types of cancer.
What happens next?
Cancer Prevention Action Week is just the start. We want to spark an ongoing national debate: with friends, family – and within government – about alcohol and cancer so that everyone can make more informed choices about their health.
But the UK government has said it won’t include mandatory comprehensive restrictions on alcohol marketing in its 10-year Health Plan – despite these being a proven, cost-effective way to reduce alcohol harm.
This is hugely disappointing. Contact the Prime Minister to make it clear that public health must be protected – and that cancer prevention cannot be sidelined.
On the blog
Media coverage
Cancer Prevention Action Week is across the news this week!
-
BBC Radio
Our Senior Policy Advisor, Kendra Chow, was invited to talk about this year’s campaign on BBC 5 Live on Saturday night. The interview was repeated across 5 Live and 43 other BBC radio stations.
-
Channel 5
Vanessa Feltz’s lunchtime show covered alcohol health warnings in a lengthy discussion including an interview with our supporter Dr Philippa Kaye.
Also on Channel 5, Jeremy Vine’s show discussed Alcohol labels should warn of cancer risk, urge health groups (The Times) in a round-up of the morning papers.
-
The Guardian
-
The Independent
-
The Times
-
The Telegraph
-
Julia Bradbury on Instagram
-
Scotland
-
International
- Mirage News (Australia)
- The Times of India
- Yahoo New Zealand
-
Science press
-
Trade press
-
Local press
- Rayo (Coventry and Nuneaton)
- This Is Wiltshire
- The Gazette and Herald
- Swindon Advertiser
- The Birmingham Mail
Facts at your fingertips
Written by experts, based on the evidence: our health resources unmuddle the myths about alcohol and cancer.
World Cancer Research Fund has responded to the UK government’s first multi-year spending review, where the Chancellor, Rachel Reeves, set out departmental budgets over the next 3 years.
Under their Health Mission, the government has committed to shifting from sickness to prevention, affirming that prevention is better than cure. This spending review marks a critical opportunity for the government to set out their investment to this commitment.
In this review, the Chancellor committed:
- £29bn for the day-to-day spending of the NHS to 2028–29.
- £80m per year for tobacco cessation programmes and to support the delivery of the Tobacco & Vapes Bill.
- £10bn in NHS technology and digital transformation by 2028–29.
- £22.6bn per year for research and development by 2029–30, including medical research.
Responding to the spending review, World Cancer Research Fund’s Executive Director of Research and Policy, Dr Giota Mitrou, said:
Today the Chancellor reaffirmed Labour’s Health Mission, including their commitment to shift from treatment to prevention. 40% of all cancer cases are preventable: as leading experts in cancer prevention, we know that primary prevention remains the most sustainable and cost-effective way to tackle cancer and other non-communicable diseases.
For example, while we are glad to see that the government will be investing £80m per year to tackle tobacco, we need to see similar efforts applied to obesity and alcohol. The expansion of free school meals is a step in the right direction and the type of action we hope to see in the upcoming 10-year Health Plan.”
Alcohol is a proven risk factor for 7 cancer types, and our evidence clearly shows there is no safe level of consumption when it comes to preventing cancer. Each year 17,000 people – 46 people every day – are diagnosed with a cancer caused by alcohol.
Alcohol deaths in England reached nearly 10,500 in 2023, a massive 42% increase since 2019. Despite these tragic statistics, alcohol policy across the UK remains woefully inadequate, doing very little to mitigate its significant harms, including cancer, and the immense burden it places on the NHS.
Making the case for change
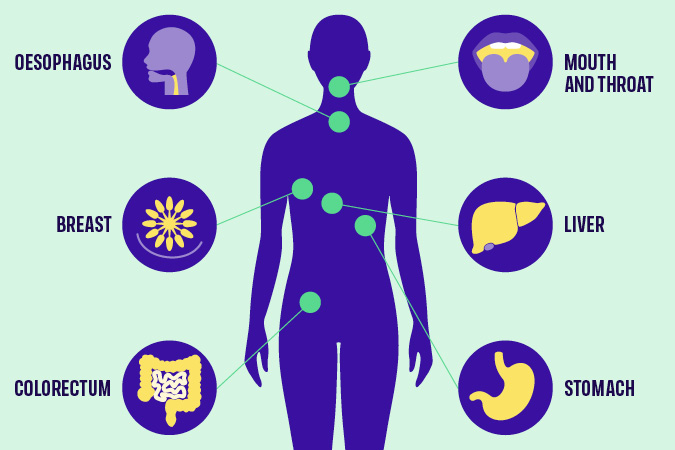
Which cancers are linked to alcohol?
That’s why this year, our flagship campaign – Cancer Prevention Action Week – focuses on the links between alcohol and cancer, aiming to ensure that everyone can make informed decisions about their alcohol consumption. While raising awareness is important, it must be combined with evidenced-based polices that enable and support people to make healthier choices.
As many aspects of alcohol policy are the responsibility of the devolved administrations, Northern Ireland, Scotland and Wales all have alcohol strategies in place. In contrast, England has not had a National Alcohol Strategy since 2012.
We’re calling on the UK government to introduce a long overdue National Alcohol Strategy for England without delay. The Strategy must introduce policies on labelling, pricing and marketing – 3 interventions that have strong evidence of positive impact. Crucially, it must also remain independent of industry influence.
1) Labelling
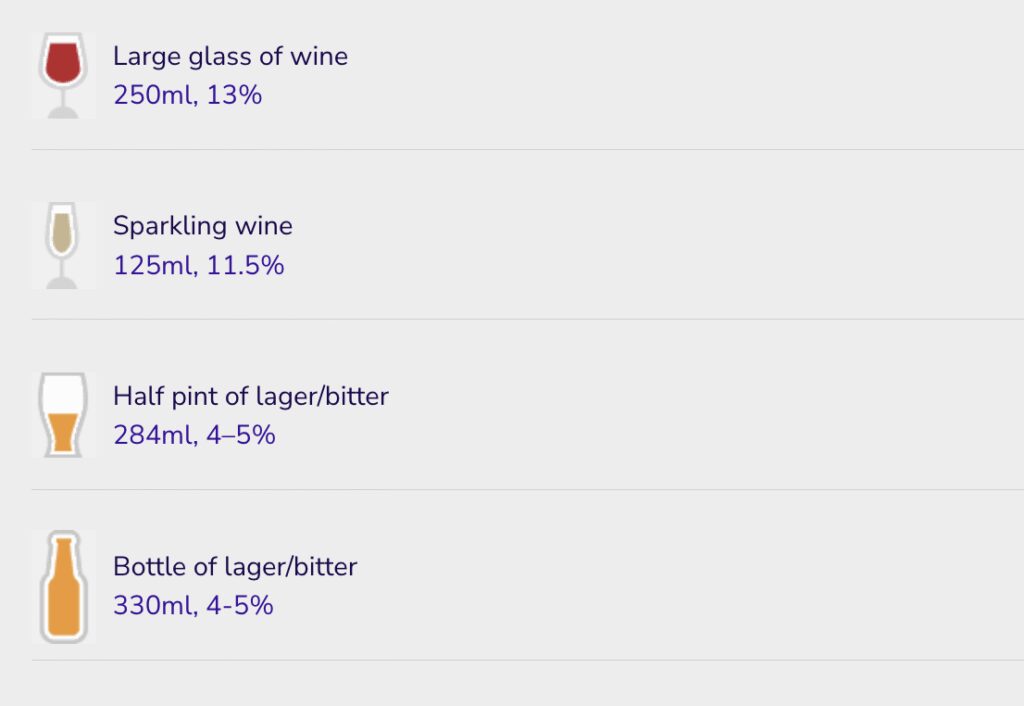
Despite being carcinogenic, alcohol is exempt from mandatory health warning labels. Unlike other food and drinks, alcohol labels are also not required to include information on nutritional content or calories. As the Alcohol Health Alliance puts it, there is more product information on a bottle of orange juice than on a bottle of beer. In fact, alcoholic drinks only have to display to display minimal information such as the name, strength as alcohol by volume (but only if over 1.2%), allergen information and the best before date (if the drink’s strength is under 10%). Even pregnancy and drink driving warnings are voluntary.
Consumers have a right to know about every product’s health risks and harms. Introducing health warning labels on alcohol that highlight cancer risk, alongside information on nutrition and calories, is an easy and effective way to ensure this. Evidence shows that effective labelling can prompt behaviour change and lead to reduced consumption.
For labelling to be effective, it must be clear, plain, distinct and mandatory. Additionally, labels should not include ambiguous language such as “drink responsibly”. Our policy position on alcohol explains that the use of QR codes to link to health information must be prohibited as, rather than informing people about risks, they provide marketing opportunities by redirecting consumers to producers’ websites.
2) Pricing
Minimum Unit Pricing (MUP) has been introduced in Scotland and Wales, but not in England or Northern Ireland. It sets a baseline price at which a unit of alcohol can be sold and targets cheap, strong alcohol that is often consumed by adolescents and other vulnerable groups.
Public Health Scotland’s review indicates that MUP has reduced alcohol-specific deaths by 13% and averted over 800 hospitals admissions every year since its introduction in 2012. MUP was found to have the most impact on those living in the 40% most deprived areas of Scotland, helping to reduce health inequalities. The Welsh government has also seen the benefits of MUP, which it introduced in 2020. Northern Ireland has consulted on proposals to introduce MUP.
England must follow suit, introducing MUP at 65p and adjusted for inflation thereafter. Without MUP in England, a 2.5 litre bottle of cider containing 19 units of alcohol can be bought for as little at £5.25. Under a 65p minimum unit price, this would rise to £12.19. Industry opposes MUP, arguing that it would damage sales in pubs and restaurants. However, most alcohol sold in these settings is already above minimum unit prices.
3) Marketing restrictions
Marketing restrictions on alcohol remain woefully inadequate. Advertising regulations prohibit linking alcohol with youth, irresponsible behaviour or social success, but enforcement is ineffective. The Advertising Standards Agency has no power to issue fines or sanctions, and often rules on complaints only after a campaign has ended. Like labelling, advertising is not a devolved issue, meaning the picture across the UK is largely the same.
Alcohol advertising is widespread, despite strong evidence linking exposure to alcohol marketing with young people drinking more and at an earlier age. The UK’s insufficient restrictions must be addressed by classifying alcohol as an “unhealthy product” under high fat, sugar or salt (HFSS) marketing restrictions. This would limit its promotion, particularly to vulnerable populations including children and adolescents.
The time to act is now
No family should have to endure the devastating trauma of alcohol-related cancer. Yet, as a result of the rise in high-risk drinking since the coronavirus pandemic, the UK could see more than 18,000 additional cancer cases by 2035.
Join us this Cancer Prevention Action Week to demand action. Sign and share our petition today, calling for a National Alcohol Strategy for England.
- The Alcohol Health Alliance, which we are a member of, has more information on MUP, labelling and marketing restrictions.