Donor power in action: 19 new research awards taking on cancer before and after diagnosis

Donations from our fantastic supporters are smartly invested into the most impactful opportunities in science, guided by our wide network of independent leading experts.
Each year, millions of people hear the words “you have cancer” – and millions more are quietly edging towards a preventable diagnosis because of factors like diet, weight, inactivity or environmental exposures.
There’s a huge opportunity here: we know that 40% of cancer cases could be prevented. But there are still major gaps in the evidence that our latest round of awards will help to fill.
The three charities – World Cancer Research Fund, the American Institute for Cancer Research and Wereld Kanker Onderzoek Fonds – have funded 19 grants through our Regular Grant Programme (12 awards) and INSPIRE Research Challenge (7 awards), backing researchers who are pushing the boundaries of what’s possible in cancer prevention and cancer survivorship.
In total, £5,115,693.43 will be awarded from our network to projects led from 9 countries across the world. Of these 19 awards:
- 12 (63%) are focused on preventing cancer
- 7 (37%) are focused on helping people live better and longer after cancer
These grants range from global cohort studies using cutting-edge ‘omics’ technologies, to clinical trials testing exercise during chemotherapy, to innovative lifestyle interventions that survivors can use right now.
This year, their specific interests span everything from microplastics and air pollution, to insect-based fibre, ultra-processed foods in childhood, and exercise woven into cancer treatment.
Rethinking what’s on our plates (and in our environment)
Food, drink and environmental exposures are shaping cancer risk in ways science is only beginning to understand. Several of our new projects are tackling this head-on.
- Hidden DNA ‘typos’ in food and bowel cancer
At the University of Oxford, Professor Skirmantas Kriaucionis is investigating whether modified DNA building blocks can ‘sneak’ into our cells and damage our DNA, increasing the risk of bowel cancer. If certain cooking methods or ingredients generate these building blocks, this research could ultimately help people – and food producers – make safer choices. - Wholegrains vs refined grains across 20 cancers
At the Cancer Registry of Norway, Dr Dagfinn Aune is using data from more than 480,000 people to understand how whole grains and refined grains affect the risk of 20 different cancers. The findings will help show how many cancers might be prevented if more people swap refined grains for wholegrain options. - Sugar, soft drinks and pancreatic cancer
At the University of Padova, Dr Alessandro Carrer is exploring how fructose from sugary drinks may fuel early pancreatic cancer development. By pinpointing this pathway, the team hopes to clarify whether cutting back on certain sugary drinks could lower risk and inform future prevention strategies. - Ultra-processed foods in childhood and lifetime cancer risk
At Murdoch Children’s Research Institute, Dr Sherly (Xueyi) Li is leading the first comprehensive study to estimate how much ultra-processed food children are eating in Australia and 25 European countries, and how this might impact their future cancer risk. This project aims to provide crucial evidence for dietary guidelines and policies aimed at protecting children from unhealthy food environments. - Microplastics, air pollution and colorectal cancer
At IFOM in Milan, Dr Vito Amodio is asking whether microplastics, nanoplastics and tiny air pollution particles (like PM2.5) contribute to colorectal cancer by driving inflammation and disrupting the immune system. The results could inform both environmental policy and personal risk reduction. - Reducing colorectal cancer risk with cricket powder and chitin
At the University of Almeria, Dr Carmen Rodriguez Garcia is exploring whether chitin, a dietary fibre found in cricket powder, can help protect the bowel. By analysing samples from a completed dietary trial, the team will see how chitin affects gut bacteria, inflammation and chemical tags on DNA in the colon – all early warning signs for colorectal cancer. This innovative project links sustainable diets with cancer prevention and could inform future trials and dietary guidance.
Protecting people where the burden is highest
Cancer prevention isn’t just a high-income country issue. Several of our new awards are designed to address urgent evidence gaps in regions where the burden is particularly severe.
- Mycotoxins, infections and Burkitt lymphoma in African children
At IARC, Dr Rita Khoueiry is investigating how mycotoxins – toxic substances produced by moulds in staple foods – and Epstein-Barr virus combine to cause Burkitt lymphoma, a fast-growing childhood cancer in sub-Saharan Africa. By following a mother-child cohort from pregnancy and analysing biological samples over time, this work aims to identify modifiable risk factors and lay the groundwork for prevention strategies that protect children now and in future generations. - Oesophageal cancer precursors in the African Oesophageal Cancer Corridor
At IARC, Dr Valerie McCormack is leading a community-based study in Malawi to understand how dietary N-nitrosamines – carcinogens found in some traditional foods and drinks – and other lifestyle factors contribute to early changes in the oesophagus that can precede cancer. By identifying high-risk exposures, this work can inform local prevention strategies in one of the world’s highest-risk regions.
These projects are about levelling the playing field so that advances in cancer prevention benefit people everywhere – not just those living in wealthier countries.
Turning treatment time into healing time
Six of our new awards are focused on cancer survivorship – helping people with cancer live longer, better lives by embedding lifestyle support into care.
- Exercise during chemotherapy infusion for metastatic colon cancer
At the University of Sydney, Dr Kate Edwards is testing a simple but powerful idea: what if patients cycle on a stationary bike during their chemotherapy infusion, instead of sitting still. The EXERTION-mC trial will test whether this approach can improve tumour response, side effects and quality of life for people with metastatic colorectal cancer. - Exercise during immunotherapy for melanoma
At Australian Catholic University, Dr Eva Zopf is investigating whether a structured exercise programme is safe and feasible during adjuvant immunotherapy for people with melanoma – and whether it can improve side effects, wellbeing and immune responses. With immunotherapy now used widely for many cancers, this work could help shape future exercise-oncology recommendations. - Long-term benefits of exercise in metastatic breast cancer
At UMC Utrecht, Professor Anne May is following up participants from the large PREFERABLE-EFFECT trial to see whether the benefits of a 9-month supervised exercise programme – such as less fatigue and better quality of life – can be sustained 2–3 years later. Understanding long-term impact and cost-effectiveness is vital for integrating exercise as part of standard care for metastatic breast cancer. - Better sleep and support for people with primary brain tumours
At the University of Sydney, Dr Megan Jeon is testing telehealth group cognitive behavioural therapy for insomnia (CBT-I) for people living with primary brain tumours. Sleep problems are common and debilitating in this group yet often go untreated. This feasibility study will explore whether CBT-I, which is the gold standard nonpharmacological treatment, can safely improve sleep, mood and daily functioning in a population that has been largely overlooked in survivorship research. - Integrated lifestyle programme for cancer survivors
At the University of Colorado, Dr Emily Hill is developing and testing an integrated nutrition and exercise programme for post-treatment survivors that also includes sleep education, stress management and wearable technology such as smart watches and connected scales. By tracking stress, immune markers and behaviour change together, the study aims to show how lifestyle interventions improve health – and how to design programmes that survivors value and actually use. - Dietary fats and response to lung cancer immunotherapy
At the University of Torino, Professor Chiara Riganti will map “good” and “bad” fats in non-small cell lung cancer tumours to see which lipid patterns predict response to immunotherapy. The team will then test whether diets rich in “good” (mono- and poly-unsaturated) fats can boost treatment effectiveness in advanced laboratory models – enhancing immunotherapy and exploring other potential health benefits. - Balancing protein and fibre to support bowel cancer treatment
At Wageningen University, Dr Dieuwertje Kok is studying how the balance of protein and fibre in the diet affects recovery and long-term outcomes for people with bowel cancer. Using data from over 2,100 participants in the COLON study, plus a new dietary intervention, the team will examine how different combinations of protein and fibre relate to treatment complications, cancer recurrence and blood markers. The findings will help shape practical nutrition programmes to support patients through treatment and beyond.
Cracking the biology that links lifestyle to cancer
Several grants are focused on understanding how lifestyle factors ‘get under the skin’ to influence cancer risk, progression and response to treatment.
- Thyroid hormones, lifestyle and liver cancer risk
At IARC, Dr Mazda Jenab will investigate how thyroid hormone metabolism and lifestyle combine to influence liver cancer risk, using large international cohorts and genetic data. - Metabolic health, blood proteins and lifestyle-related cancers
At IARC, Dr Komodo Matta will use proteomics (large-scale protein profiling) to understand how metabolic health drives a range of lifestyle-related cancers – and identify blood protein signatures that could become targets for prevention. - Body composition, inflammation and multiple myeloma
At the University of Bristol, Dr Lucy Goudswaard will explore how body fat distribution and inflammation influence the development of multiple myeloma from its precursor condition, MGUS, helping to identify high-risk individuals and new intervention targets. - Exploring selenium and lung cancer risk
At the University of Southern Denmark, Professor Paolo Ceppi is investigating how selenium, a dietary mineral found in foods like nuts, meat and grains, influences the development of non-small cell lung cancer. By combining advanced lab studies with analysis of long-term selenium intake human populations, the goal is to provide clear, evidence-based guidance on selenium intake that could help reduce the burden of this deadly disease.
Together, these projects will help turn broad advice like “improve metabolic health” into precise pathways and actionable strategies.
Why this matters – and how donors make it possible
All of this science has one simple goal: fewer people getting cancer, and better lives for those who do.
From children growing up surrounded by ultra-processed foods and environmental pollutants, to adults at high risk of bowel, liver, pancreatic or oesophageal cancer, to people navigating life with metastatic breast cancer, brain tumours, melanoma or myeloma
These 19 projects are designed to produce the kind of robust, practical evidence that changes guidelines, shapes policy and transforms care.
None of it would be possible without the generosity of people and organisations who choose to support our work. Every donation – whether it’s a monthly gift, a legacy in a Will, or a fundraising challenge – helps us award more of this high-impact, prevention and survivorship-focused research. Thank you for supporting us.

Be the first to know
Want to be kept fully up-to-date with our research findings? Or learn more about our work helping people living with cancer?
Full list of research grants
Regular Grant Programme
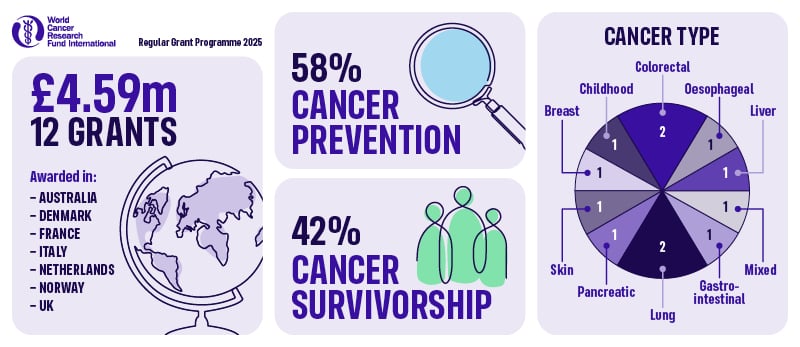
1. Professor Anne May, University Medical Centre (UMC) Utrecht (UCMU), the Netherlands: Long-term effects of exercise on quality of life in patients with metastatic breast cancer: a follow-up study of the randomized PREFERABLE-EFFECT study – £224,213.65
2. Professor Paolo Ceppi, University of Southern Denmark, Denmark: Exploring Selenium and Lung Cancer Risk – £384,944.00
3. Dr Dagfinn Aune, Cancer Registry of Norway, Norway: Whole grains and refined grains and cancer incidence: habitual intakes, changes in intakes, substitutions and risk of 20 cancers in four Scandinavian cohort studies and a large American multiethnic cohort – £500,000.00
4. Dr Dieuwertje Kok Wageningen University, the Netherlands: Balancing dietary protein and fibre intake to improve outcomes of colorectal cancer treatment £464,411.00
5. Dr Rita Khoueiry, International Agency for Research on Cancer (IARC), France: Studying the impact of in-utero and early life exposure to mycotoxins on viral infections and the epigenome: unveiling the risk factors of endemic Burkitt Lymphoma in African children – £498,285.25
6. Dr Valerie McCormack, International Agency for Research on Cancer (IARC), France: Diet, N-nitrosamines and Esophageal Squamous Cell Carcinoma precursors in the African Esophageal Cancer Corridor: EndoSCCAPE – A community-based cross-sectional study in Malawi – £413,400.00
7. Professor Skirmantas Kriaucionis, University of Oxford, United Kingdom: Modified Nucleic Acids in Diet and Bowel Cancer Risk – £489,531.32
8. Dr Mazda Jenab, International Agency for Research on Cancer (IARC), France: Investigating the Role of Thyroid Hormone Metabolism in Liver Cancer Development: Integrating Lifestyle and Omics Data from Large Cohort Studies (HepaThyroid-omics) – £498,196.61
9. Dr Kate Edwards, University of Sydney, Australia: EXERTION-mC: EXERcise during chemoTherapy infusION to improve outcomes for people with metastatic Colon cancer – £499,242.00
10. Dr Alessandro Carrer, University of Padova, Italy: Interrogating the impact of fructose-to-acetate conversion for nucleolus organization and pancreatic cancer predisposition – £500,000.00
11. Dr Eva Zopf, Australian Catholic University, Australia: Safety and feasibility of exercise in patients with melanoma undergoing adjuvant immunotherapy with immune checkpoint inhibitor therapy – £59,519.00
12. Professor Chiara Riganti, University of Torino, Italy: Polyunsaturated fatty acids improve immunotherapy efficacy in non-small cell lung cancer – £60,000.00
Inspire Research Challenge
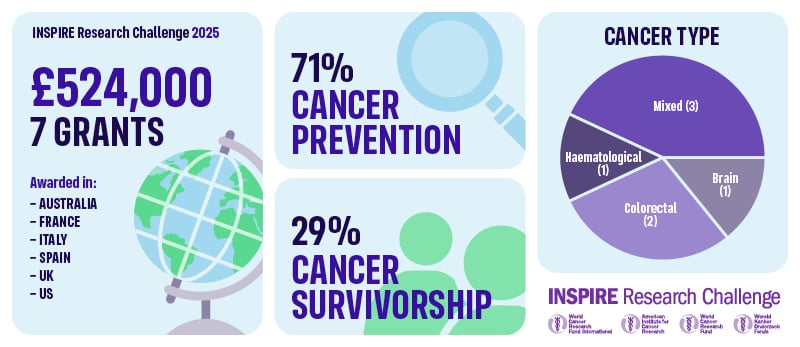
13. Dr Carmen Rodriguez, Garcia University of Almeria, Spain: Reducing Colorectal Cancer Risk with Cricket Powder and Chitin: Analysis of Epigenetic and Inflammatory Biomarkers from a Randomized Controlled Trial – £75,000.00
14. Dr Lucy Goudswaard, University of Bristol, United Kingdom: Characterising the role of body composition and inflammation in multiple myeloma – £74,950.60
15. Dr Komodo Matta, International Agency for Research on Cancer (IARC), France: Understanding the role of metabolic health in lifestyle related cancers through proteomics – £74,100.00
16. Dr Sherly (Xueyi) Li, Murdoch Children’s Research Institute, Australia: Ultra-processed food intake in childhood and their link to future risk of cancer – £75,000.00
17. Dr Vito Amodio, IFOM ETS – The AIRC institute of Molecular Oncology, Italy: Dissecting the impact of exposure to environmental pollutants on chronic inflammation and colorectal cancer onset – £74,900.00
18. Dr Megan Jeon, University of Sydney, Australia: A phase II single-arm feasibility study of telehealth group cognitive behavioural therapy for insomnia (CBT-I) in adults with primary brain tumours using a novel online platform for a stepped clinical pathway for sleep disturbance – £75,000.00
19. Dr Emily Hill, Regents of the University of Colorado, United States: Impact of an integrated nutrition and exercise program for post-treatment survivors on sleep quality, perceived stress, and biomarkers of immune dysregulation – £75,000.00



