We spoke to Dr Renate Winkels (pictured) and Dr Laura Winkens, at Wageningen University & Research, to discover more about their studies in bowel (also known as colorectal) cancer.
We spoke to Dr Renate Winkels (pictured) and Dr Laura Winkens, at Wageningen University & Research, to discover more about their studies in bowel (also known as colorectal) cancer.
Your team looked at what influences people’s health behaviours after they’ve been treated for bowel cancer. What do you mean by health behaviours and what did you find out?
Health behaviours are the everyday choices people make that affect their health. In this study, we focused on 2 things:
- healthy eating (more fruit, vegetables, whole grains and beans; and less fast food, red meat, processed meat, sugary drinks and alcohol)
- physical activity
For people who’ve had bowel cancer, healthy behaviour may be associated with living longer, feeling better and having fewer problems like fatigue.
However, in previous studies, we found that many bowel cancer survivors don’t make big changes after treatment. Survivors are dealing with side-effects from the cancer or its treatment (such as gastrointestinal problems, fatigue or body image distress), which can make it hard to eat well and stay active.
Our study looked at what helps or gets in the way of healthy behaviour for people who have finished treatment for bowel cancer. We found:
Personal factors matter
How much time people have, their motivation, what they believe about healthy habits, what they know, and the skills they have can all influence whether they eat well and stay active.
Support helps
Encouragement and support from family and friends, or feeling like healthy habits are normal in their social circle, can make a big difference.
Environment plays a role
Access to gyms, parks, or even just good weather can affect how easy it is to be active.
Cancer symptoms can get in the way
Ongoing physical issues after cancer treatment, like fatigue or bowel problems, often make it harder for people to stick to healthy habits. But if someone is feeling physically well, they’re more likely to eat better and stay active.
Mental health may be important
Depression or being unhappy with one’s body seem to be linked with less healthy behaviour.
In short, to help people with bowel cancer lead healthier lives after treatment, we need to focus on motivation, knowledge, support, and overcoming the challenges they face physically and emotionally.
Towards a more complete picture
Your team conducted a “systematic review”. What is that and why is it important?
We wanted to find out what other scientists had studied, so we could build our study on the latest evidence. Moreover, we wanted to provide an overview of the topic. We looked at 21 papers, but we started with around 800 publications, and had to sift through them to identify the relevant ones.
You divided the studies into quantitative or qualitative. Why did you choose to look at both?
Quantitative studies collected a lot of numbers and measurements. The studies used standardised questionnaires to collect data on dietary intake and other aspects of lifestyle. Those studies answer questions like “how many” or “how much”.
Qualitative studies focus more on experiences. Such studies are mostly interviews to better understand why people do what they do, or how people behave.
Together, they provide a richer, more complete picture of the challenges and motivations colorectal cancer survivors face.
Were you surprised that people find it hard to change their behaviour?
Not really. Most people will recognise how challenging it can be to always make healthy choices. After cancer, when you’re rebuilding your life, that can be even harder.
How important is mental health for people living with and beyond bowel cancer?
Mental health is a very broad topic. People who have had bowel cancer may have a stoma, or be suffering from fatigue, or from bowel functioning problems. These can have a real impact on your life, and it’s important to address them. Some care teams really have an eye on this, but it’s not always the case. One patient told me that she did not dare to discuss her feelings of severe fatigue with her oncologist, as the oncologist told her that “fatigue was not a thing” for people with bowel cancer. We need more awareness and integrated care that addresses both mental and physical health to truly support survivors’ wellbeing.
You’ve also looked at whether following our Cancer Prevention Recommendations can reduce fatigue for people with bowel cancer.
We set up a study to assess whether following the Recommendations would help people to feel less fatigue. Cancer-related fatigue is a symptom that many bowel cancer patients experience during treatment and after completion. What is disturbing is that this type of persistent, overwhelming sense of physical, emotional or mental fatigue is not proportional to activity nor relieved by resting or sleeping.
We recruited participants for the trial who were experiencing cancer-related fatigue. In a randomised study, half of the group received lifestyle coaching to improve their adherence to the Recommendations, while the control group did not.
The coaching really helped the participants to adopt a healthier lifestyle: over time, this group reported eating more fruit and vegetables, and less processed meat and sugar-sweetened beverages. Also, physical activity levels went up more in the group that received coaching than in the control group.
Nevertheless, those changes didn’t result in less fatigue. This suggests that while these changes have many benefits, managing fatigue may require additional, targeted interventions.
This grant was funded by Wereld Kanker Onderzoek Fonds based in the Netherlands, as part of the World Cancer Research Fund International network.
Key takeaways:
- The CO21 CHALLENGE Trial found that a structured exercise programme after chemotherapy led to a 28% lower risk of cancer recurrence in colon cancer survivors compared with usual care.
- This is the first randomised controlled trial (RCT) to show that exercise directly improves survival in colon cancer patients. It confirms what observational studies have long suggested.
- The results were presented at a recent conference and made headline news. Experts say the CHALLENGE Trial marks a shift from viewing exercise as a “nice to have” to a “need to have” in cancer care.
Colon (part of the large bowel) cancer survivors who took part in a 3-year structured exercise programme had a 28% lower risk of cancer recurrence or a 2nd cancer. They also had a 37% lower risk of death compared with usual care.
These findings were shared at the 2025 Association of Clinical Oncology (ASCO) Annual Meeting. They were also published in the New England Journal of Medicine.
The ASCO Annual Meeting is the world’s largest oncology conference. It attracts more than 40,000 attendees from around the world. Every year, ASCO highlights the latest advancement in treatments. It also shares the directions that have the greatest potential for progress and patient impact.
Spotlight on exercise
The CO21 CHALLENGE Trial pulled back the curtain on a weapon that has been hiding in plain sight: physical activity. The results of the trial showed improvement in disease-free survival and overall survival in colon cancer survivors in the aerobic exercise intervention group. This trial is the first gold standard RCT to show what has long been indicated from observational studies. This is a big deal!
The impact of exercise on cancer outcomes has been a topic of great debate. Observational research has shown improvements in survival and quality of life linked to higher levels of physical activity. However, observational study designs are limited. They do not show cause and effect.
Plus, they are hard to implement in clinical settings due to concerns that the reported effects may not truly reflect the impact of exercise (and may be due to something else).
Our research
Over the past few years, World Cancer Research Fund International has done extensive reviews through its flagship Global Cancer Update Programme (CUP Global).
CUP Global includes partnerships with American Institute for Cancer Research, World Cancer Research Fund in the UK and Wereld Kanker Onderzoek Fonds in the Netherlands.
Our CUP Global reviews look at the extent to which diet, nutrition and physical activity impact people after a diagnosis of breast and colorectal cancers with regard to:
- cancer-specific mortality
- all-cause mortality
- risk of cancer recurrence
- health-related quality of life
An expert panel judged the strength of this CUP Global evidence. There were some limitations. Still, detailed recommendations were made to strengthen future research. One of the key recommendations was for well-conducted trials to look at the impact of nutrition or physical activity. The CHALLENGE trial is therefore very timely.
The CUP Global analysis was published in the International Journal of Cancer. It was cited several times in the CHALLENGE trial manuscript.
The CUP Global analysis compared highest with lowest levels of activity. We found that all-cause mortality was reduced by 23–40% depending on physical activity exposure.
Prof Anne May, University Medical Centre, Utrecht
During our review of the literature concerning the impact of post-diagnosis physical activity on colorectal cancer prognosis for the Global Cancer Update Programme (CUP Global), we were unable to draw strong conclusions due to lacking evidence from randomized controlled trials. The Challenge trial provides exactly the evidence we were waiting for.
The summary estimate for studies that assessed activity dose was measured in MET hours per week.
- A 10 MET hour per week increase in activity was linked to a 24% reduction in all-cause mortality.
- A change of 10 MET hours per week was also the intervention goal in the CHALLENGE trial.
The effect sizes in this first, gold-standard RCT are remarkably well-aligned with the CUP Global analyses of observational studies.
During the presentation of the trial results at ASCO, the authors shared this chart. It includes the treatment benefits from approved therapies for colon, lung and breast cancer.
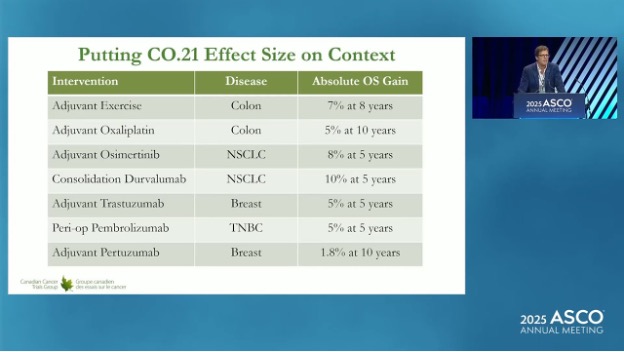
With 7–8% gains, you can see that exercise compares very favourably with other approved therapies in terms of absolute overall survival gain.
Collecting clinical trial evidence
The CHALLENGE trial confirms the clinical benefits that had been reported from observational studies. However, previous RCTs have also hinted at the accuracy of the results from observational studies. For example:
- The LEANer trial was published in 2023. It showed that triple negative breast cancer patients randomised to a diet and physical activity intervention before chemotherapy had a 53% higher rate of treatment success (eliminated cancer cells).
- A trial published in June 2025 showed that an exercise programme during and after chemotherapy increased the immune system responses in oesophageal cancer patients.
World Cancer Research Fund will fund the Optimus trial in the UK. Dr David Bartlett and Prof Adam Frampton at the University of Surrey will lead this study. It was proposed due to these findings.
Next steps
Dr Kerry Courneya co-led the CHALLENGE trial. At ASCO, he said these results could change practice for high-risk stage 2 and stage 3 colon cancer.
He expressed reservation that these results could be generalised to other sites and cancer stages. But he was optimistic that similar trials could be done more quickly than the CHALLENGE trial by taking advantage of newer methods. This could include using remote exercise assessments or activity trackers.
Dr Courneya noted that “support from funding agencies like WCRF/AICR is critical to moving this field forward because of limited access to funding for lifestyle research”.
AICR recently funded a project linked to the CHALLENGE Trial. It is led by Dr Kristin Campbell at the University of British Columbia in Canada. It will look at how muscle and fat tissue respond to exercise and how that may contribute to the observed survival benefits.
The response to the CHALLENGE Trial has made media headlines. Cancer researchers, doctors and patients are also excited by the news. This suggests that adding exercise as an additional part of treatment will gain further momentum.
While more trial data will be needed to support broader implementation, we are likely leaving the “nice to have” approach to exercise oncology and entering the “need to have” phase!
Research grants on physical activity
A selection of some of the grants we have funded that focus on the impact of physical activity on people living with and beyond a cancer diagnosis.
Researchers funded by World Cancer Research Fund have discovered that brisk walking is linked to a lower risk of 5 cancers:
- anal
- liver (hepatocellular carcinoma)
- small intestine
- thyroid
- lung
Using information stored in the UK Biobank – a large database of many different aspects of health – scientists explored the link between walking pace – slow, steady or brisk – and the risk of developing 28 types of cancer.
They confirmed that the link between brisk walking and a reduced risk of developing the 5 cancers was true, even after accounting for overall physical activity and total walking time.
Speeding up your walk could represent an easy, low-cost public health intervention to decrease cancer risk.
The paper, published in BMC Cancer, says:
“Adopting a brisk walking pace may represent a pragmatic target for public health interventions to decrease cancer risk, particularly in circumstances where increases in walking volume or frequency prove impractical.”
PhD student Michael Stein’s research was supported by funding from Prof Michael Leitzmann’s grant. This research was funded by World Cancer Research Fund as part of the WCRF International Regular Grant Programme.
> Read the full paper: Usual walking Pace and risk of 28 cancers– results from the UK biobank
 John Steventon is our very own supporter superhero. He completed a HYROX in December dressed as comic book character Wolverine, alongside a friend who dressed as Deadpool – and he isn’t stopping there.
John Steventon is our very own supporter superhero. He completed a HYROX in December dressed as comic book character Wolverine, alongside a friend who dressed as Deadpool – and he isn’t stopping there.
HYROX is an indoor fitness race enhanced by workout stations along the route, so competitors run 1km, then do a workout – 8 times! The workouts include rowing, pulling and pushing a sled, and lunges while carrying a sandbag, making it an exhausting but fun challenge.
John said: “Everything I’ve done in life, I’ve wanted to share with others. As a DJ, I taught aspiring musicians and even wrote DJing for Dummies. In my TV career, I mentor new editors. When I was racing in indoor rowing, I launched the RowAlong YouTube channel to help home rowers stay motivated. So, when I started competing in HYROX, I wondered how I could use this platform to make a difference. “
“I knew I’d never be a podium finisher, but after my skin cancer diagnosis, I found a purpose: racing as Wolverine to raise money for World Cancer Research Fund. The response from the HYROX community has been incredible – not just in donations, but in the conversations I’ve had. Nearly everyone I meet has been touched by cancer in some way, whether personally or through friends and family.”
‘I thought I was invincible’
“Even though the doctor said, “Don’t worry”, when I heard the words “That’s skin cancer” the last hope that I was indestructible fizzled away. I’d always thought I was invincible – after all, I like to dress up as Wolverine – but skin cancer reminded me that none of us are.”
John’s diagnosis helped him become more aware of the importance of cancer prevention. “I remember being 7 years old, resisting my Mum’s attempts to put sun cream on me. I often opted for the lowest SPF possible, thinking sunburn was just a fast track to a tan. Coming from Scotland, where sunshine is a rarity, I’ve always craved the sun’s warmth. But now, I never go without factor 30 or 50. If only I had learned that lesson earlier.
“The guidance from the World Cancer Research Fund has been invaluable in helping me understand the importance of proper nutrition and lifestyle choices in cancer prevention and overall health. Exercise alone isn’t enough – we need to fuel ourselves properly and protect ourselves from preventable risks like excessive sun exposure.”
John continues to take on HYROX challenges to raise money for us. He’s completed 3, including one in Frankfurt, and is running The Grid competition again in September, as well as more HYROX events this year. So far, he’s raised nearly £2,000 towards cancer prevention – thank you, John!
In almost every region of the world, overweight and obesity among children and adolescents is a public health problem. There has been no progress in stemming the rate of overweight and obesity in children under 5 years in nearly 20 years, according to the World Health Organization (WHO).
This is a problem, because we know that when people live with overweight or obesity near the start of their lives, it often becomes a challenge throughout their adult lives.
What’s the problem with being inactive?
Young people may not be thinking very much about their risk of developing cancer. But the habits laid down in youth can last a lifetime. Our evidence shows that being active reduces the risk of colon (part of the bowel), post-menopausal breast and womb cancers.
Perhaps more importantly, being physically active also helps reduce our risk of living with overweight and obesity – a cause of at least 13 different types of cancer. Put simply, excess weight results from an imbalance between the energy we take in through our diet, and the energy we expend through being active (and other bodily functions). While we need to consider wider issues related to our ability to access a healthy diet, and managing stress and sleep levels, part of the solution involves being more active.
Are screens a particular problem?
Screens, and particularly mobile phones, have been blamed for a range of social and health problems among young people, including:
Evidence from our 2018 Diet and Cancer Report revealed convincing evidence that more screen time for children (from mobile phones but also using computers at school and watching devices during leisure time) makes weight gain more likely, as well as overweight and obesity.
The reasons for this are mixed. We tend to watch screens while sitting down, which uses less energy. Watching screens can also encourage us to eat more than is needed, not least because of exposure to adverts for unhealthy food and drinks, which young people may be particularly susceptible to.
The WHO lists limiting screen time as one of the ways to prevent and manage overweight and obesity in young people – but it’s only one.
What are the barriers to getting more active?

Young people’s experiences differ but, looking at the evidence and talking to parents and teenagers in the UK, a few common problems are highlighted:
- Underfunded / poor-quality equipment in public spaces (that may also feel unsafe to use).
- Cost – young people often don’t have a steady income, and gyms/clubs/sports can be expensive. Young people need access to parks and sports fields in their neighbourhoods.
- Travel – young people are often dependent on others for travel, which makes active travel – including safe routes to walk or cycle to school – and good public transport infrastructure so important (see below).
- Lack of options – children and young people in the UK are often offered activities such as football, netball and cross-country, but many want to try out less conventional sports such as yoga, dodgeball or trampolining.
- Gender – there is a significant decline in young girls taking part in sport, and parents of girls highlighted particular barriers to participation around body image, concerns about sweating and clothing, and lack of private changing spaces.
Elsewhere, a 2022 study looking at Botswana, Ethiopia, South Africa and Zimbabwe identified barriers around funding, but also highlighted community safety and a general lack of infrastructure as challenges.
What solutions are working around the world?
When developing ideas and designing policies to tackle overweight and obesity among children and young people, one voice is often unheard – that of young people themselves. From 2018–23, World Cancer Research Fund was involved in an innovative EU-funded project called CO-CREATE, which aimed to change that by putting young people at the forefront of tackling the obesity epidemic in Europe. The youth representatives on the project came up with 4 demands to policymakers, including “Offer all children and adolescents free, organized physical activities at least once every week.”
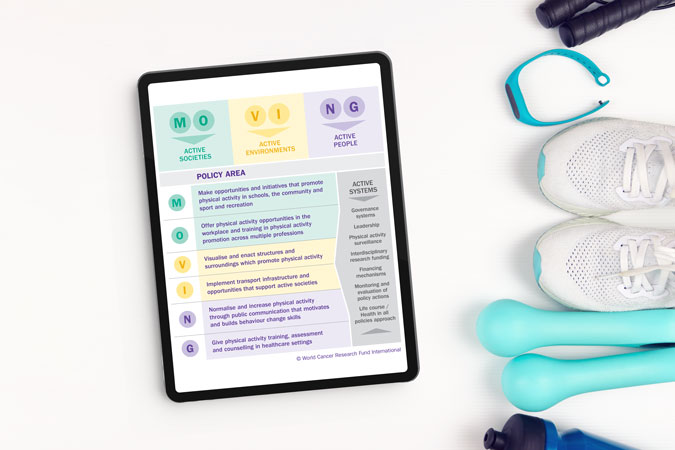
Using what they learned as part of the CO-CREATE project, our Policy team have devised a policy factsheet on physical activity, outlining the best ways to meet our Cancer Prevention Recommendation to be physically active.
Of all the information in the factsheet, some policy recommendations would specifically benefit children and young people, if acted on by governments around the world. These include:
- Initiatives that optimise opportunities for physical activity (including walking and cycling to and from school).
- Active play before and after school, as well as during recess and lunch breaks.
- Reduce sitting during classes.
- Policies to priorities active urban design, like ensuring access to open/green space or walking and cycling infrastructure where people live.
To keep people informed about both the need to be active, and the opportunities available to them, we also recommend:
- High quality physical education in school curricula.
- Enhanced physical activity training for all teachers.
And some of these innovative policies are already being undertaken in parts of the world. There are many policies recorded in our MOVING database mandating physical activity in schools, broadly ranging from 2–4 hours per week, depending on age and country.
And it’s not just dedicated PE sessions. Italy’s Scuola attiva kids aims to promote a culture of wellbeing and movement among not only students but teachers and families as well. In Finland, the Students on the Move programme encourages young people to sit less and move between breaks. Belgium’s Adventurous Activity initiative offers young people the chance to try out high and low ropes, tree climbing, rowing, BMX, skiing and orienteering.
Yet parents we spoke to suggested that there also needs to be a reframing of how PE is seen in school. One parent in Surrey, UK, said: “If you’re really good, you tend to do loads as part of a club, but there seems to be very little for those who aren’t any good.”
“There’s different aspects of sports. There’s one where you’re trying to create lifelong fitness for young people to engage in sport as part of a healthy lifestyle. And there’s another part where you need competitive sport to provide appropriate challenge” – Jennifer Cole, teacher and parent of 3, Brunei
“Emphasise fun so everyone can join in. Let people compete and win something but focus on beating personal bests rather than being top of the class so it’s not exclusive. Why not offer points or vouchers for those who increase their steps the most, not the ones with the overall highest numbers, so you’re encouraging people who don’t do anything?” – Mike, parent of 3 including 2 teenage girls, UK
Active travel was another key concern for parents – and is also one of our policy recommendations, including:
- Transport policies, systems and infrastructure that prioritise walking, cycling and use of public transport.
- Road safety actions for pedestrians and cyclists.
Active travel, which has the additional benefit of helping countries meet climate commitments, is already being promoted in many European countries. Austria’s Kindergarten Mobility Box aims to make walking and cycling the norm from a young age, and Belgium has similar scheme.
Perhaps, rather than just focusing on crisis-driven solutions to an increasingly inactive world, we need to listen more to young people about the changes they want to see in their world, alongside implementing policies that make it easier for everyone – especially young people – to move more and sit less as part of their everyday lives.
Want to get more active?
Check out our resources to help you get moving – written by experts
Siobhan McGeown
Siobhan was inspired to run by her parents (in main picture), who have both had cancer. She says: “After watching both my parents suffer from cancer (ovarian and prostate), as well as several other close family members, I want nothing more than to see better outcomes for cancer diagnoses, as well as better detection and testing before it gets to that stage.”
Angela Brooks (left, wearing cap)
 Angela was diagnosed with breast cancer in 2021 aged only 33. She’s currently in remission but still living with the impact of cancer, including early menopause. Angela told us about her training schedule: “Every 3 weeks, between rounds of chemotherapy, I set myself the goal of completing a 10k run.”
Angela was diagnosed with breast cancer in 2021 aged only 33. She’s currently in remission but still living with the impact of cancer, including early menopause. Angela told us about her training schedule: “Every 3 weeks, between rounds of chemotherapy, I set myself the goal of completing a 10k run.”
Sam Burton
 Sam says: “The decision to run for World Cancer Research Fund is driven by my Father’s recent diagnosis with kidney cancer, an event that has reshaped my perspective on life and illuminated the critical importance of cancer research and advocacy.”
Sam says: “The decision to run for World Cancer Research Fund is driven by my Father’s recent diagnosis with kidney cancer, an event that has reshaped my perspective on life and illuminated the critical importance of cancer research and advocacy.”

Jack Gibbons and family
Jack Gibbons
 This is Jack’s second marathon for us, having also run in 2018. He’s running in memory of his mum, Maggie, who received a diagnosis of very aggressive stage IV melanoma in late 2023 and passed away in January 2024.
This is Jack’s second marathon for us, having also run in 2018. He’s running in memory of his mum, Maggie, who received a diagnosis of very aggressive stage IV melanoma in late 2023 and passed away in January 2024.
Maggie was there to support Jack when he ran his first marathon and was there at the finish line of the London Landmarks half in 2023 to see him over the line. Her support meant the world to Jack and he’s proud to be able to run for her in 2025 and raise money for World Cancer Research Fund.
David Herlihy
 David sadly lost his Dad to cancer in April 2024, and his Mum has been diagnosed with cancer for the second time in 5 years. He’s dedicated to health and fitness, and has completed 5 marathons, an ironman and 2 ultra marathons.
David sadly lost his Dad to cancer in April 2024, and his Mum has been diagnosed with cancer for the second time in 5 years. He’s dedicated to health and fitness, and has completed 5 marathons, an ironman and 2 ultra marathons.
Hannah Stedman
 Hannah is running in memory of her amazing Mum, who “had a very quick battle with lung cancer in October 2023. She was diagnosed on the 3rd and had passed by the 24th. To say this experience was the hardest thing of my life is an understatement.”
Hannah is running in memory of her amazing Mum, who “had a very quick battle with lung cancer in October 2023. She was diagnosed on the 3rd and had passed by the 24th. To say this experience was the hardest thing of my life is an understatement.”
George White
 George is a mortgage broker based in the West Midlands and is motivated to run for us after recently losing his Godfather to cancer.
George is a mortgage broker based in the West Midlands and is motivated to run for us after recently losing his Godfather to cancer.
The International Agency for Research on Cancer estimates that, by 2050, the world will see 35 million new cancer cases each year, up by 15 million annual cases in 2022. Yet with the right policies to prevent cancer, 14 million of those people could avoid their diagnosis. These policies would need to address a variety of factors, including tobacco, alcohol, overweight and obesity, breastfeeding and unhealthy diet.
Cancer places increasing burden on society
As the cancer burden increases, the strain on our health systems, economies and families becomes harder to meet. Unhealthy weight – just one risk factor – is projected to cost the global economy more than $4 trillion a year by 2035. Our food systems make eating a healthier diet harder. High production and consumption of red and processed meat, and low consumption of wholegrains, vegetables, fruit and beans, plays a role in increased cancer risk and the risk of other diseases such as diabetes. This misalignment also contributes to unhealthy natural environments, as diet-related greenhouse gas emissions are significant contributors to global warming. Most of these are related to production of animal-based foods. This is why prevention is the only sustainable way forward – with resilient populations and food systems working together for public health.
Prevention the sustainable way forward
 We believe that prevention must be prioritised and is the only sustainable way forward. We also need to better explain:
We believe that prevention must be prioritised and is the only sustainable way forward. We also need to better explain:
- The science around cancer risk and diets, weight, breastfeeding, physical activity, and alcohol – as summarised in our Cancer Prevention Recommendations.
- Which policies should be prioritised to shape healthier environments that minimise these cancer risks for populations.
- How cancer prevention policy can have positive cascading effects for our health, but also for our health systems, our societies and our shared natural environment.
Cancer prevention policies can have ripple effect
We also know that cancer prevention policies can touch on and improve other areas beyond health. For example, diets high in red and processed meat increase people’s risk of colorectal cancer, and that healthier diets made up of more wholegrains, fruit and vegetables can protect people from the same type of cancer. This is why our Cancer Prevention Recommendations say people should limit red and processed meat, and eat a diet rich in wholegrains, vegetables, fruit and beansAt the same time, if our food systems produced less red and processed meat, and animal- food in general, and instead moved towards producing plant-based foods, this would have a significant impact in lowering diet-related CO2 emissions. Policymakers need to make sense of these connections, and our guidance shows what they need to do to promote such positive cycles – or co-benefits.
Why we created the Blueprint
Our well-established Cancer Prevention Recommendations cover 10 ways in which individuals can minimise their risk of preventable cancers. A growing body of evidence is showing that adherence to these Recommendations is associated with lower risk of developing cancer and other NCDs, but also lower risk of dying from cancer.
However, the Recommendations have not – until now – been presented alongside population-level policy advice. We need to promote an integrated approach to preventing cancer, otherwise policymakers may risk formulating repetitive but disconnected policy strategies across these areas that do not speak to or build on each other. For example, marketing restrictions can be a useful tool to encourage healthy diets but are also relevant for promoting breastfeeding and limiting alcohol consumption. Even though the targeted products are different, there are lessons to be learned from policy efforts across different cancer risk factors.
By joining the dots in these different areas, we can create greater awareness of how different policy approaches can contribute to cancer prevention. Our new blueprint makes a compelling case for action, especially for prevention to be included in national cancer plans. The blueprint also reinforces the need for a whole-of-government approach that puts public health goals before commercial interests.
What’s inside the Blueprint?
The Blueprint is accompanied by factsheets on specific cancer risk factors.
Our policy blueprint makes the case for population-level policy action and focuses on 5 factors: diet, weight, breastfeeding, physical activity and alcohol – in line with our Cancer Prevention Recommendations. We also look at how these factors can support people living with and beyond cancer
Our blueprint is an essential, evidence-based guide for policymakers and advocates, pulling together tools and resources to provide a comprehensive resource on cancer prevention. It pulls together existing tools and resources to support efforts on cancer prevention, including key guidance for World Health Organization, but also our existing NOURISHING nutrition and MOVING physical activity policy frameworks. All this information is distilled in a package of resources:
- An outline of 8 policy areas – including marketing restrictions, fiscal and legal, procurement, planning and incentives in communities– and how they apply to diet, weight, breastfeeding and physical activity.
- 10 factsheets with in-depth technical detail on how to roll out each Recommendation at population level.
- An exploration of the co-benefits of cancer prevention policy: addressing health inequities; meeting climate and sustainability targets; addressing commercial determinants of health; and fulfilling human rights.
- 7 strategies to help policymakers take action.
The goal of these resources is to strengthen understanding of how environment shapes cancer risk, and what policymakers can do about it.
How it was developed
To develop these resources, we built on our policy work, we reviewed existing key policy documents, and asked experts in the science and policy of cancer prevention, as well as lawyers, advocates for non-communicable disease prevention or breastfeeding what is most important in their respective areas. We then brought all the main elements together.
What’s next?
The Policy blueprint for cancer prevention will now be a centrepiece of our conversations with policymakers going forward – from Member States at the World Health Organization to the UN High-Level Meeting on Non-communicable diseases.
We invite you all to get involved: download the blueprint, share it, and use it in your work.
> Download our factsheets and other policy tools in our resource library
> To give us feedback and share how you want to use the blueprint, write to policy@wcrf.org
Achieving a balanced combination of exercise and controlling our waistline is far more effective in reducing our risk of cancer than doing just one or the other, according to a study funded by World Cancer Research Fund.
In the world’s first study looking at the effectiveness of combining these measures, we found that only doing one is not enough to lower our risk of cancer. The study, which looked at more than 300,000 people, found that:
- People not meeting World Health Organization (WHO) guidelines on waist circumference are at 11% greater risk, even if they are physically active.
- People not meeting WHO guidelines for physical exercise are at 4% greater risk, even if “abdominally lean” (ie they have a smaller waist).
- Achieving neither means a 15% greater risk.
The study – WHO guidelines on waist circumference and physical activity and their joint association with cancer risk (Lead researcher: Prof Michael Leitzmann, University of Regensburg) – was published in the British Journal of Sports Medicine.
Prof Michael Leitzman
We're excited about the insights we’ve uncovered regarding the interplay between waist circumference and physical activity in reducing cancer risk. Our findings highlight the value of addressing multiple factors together, showing that both maintaining a recommended waist size and being physically active are critical for cancer prevention. This research reinforces the importance of practical, achievable changes that can have a meaningful impact on health over time.
Dr Helen Croker
This is the first study to examine the independent and combined impact of waist circumference and physical activity levels. The findings underscore the importance of a holistic approach instead of focusing on a single factor to reduce cancer risk. Maintaining a healthy weight and, in particular, having a waist circumference within the recommended level and being physically active, along with eating a healthy diet, are all crucial steps to reduce cancer risk. People can start by making small, sustainable changes like incorporating regular movement into daily routines or choosing healthier food options.
World Cancer Research Fund has been at the forefront of cancer prevention in the UK and globally for decades. We developed Activ8, a free 8-week programme to encourage people to move more, eat well and reduce their cancer risk. Every step is backed by science and brings our Cancer Prevention Recommendations to life.
At World Cancer Research Fund, our mission is to live in a world where no one dies from a preventable cancer, so of course they’re all designed to help you live a healthier, happier cancer free life!
25 things for 2025
1. Drink more water!
The human body comprises around 60% water, so drinking enough water will help improve your physical performance and increase your energy levels.
2. Eat more beans, legumes and pulses
They’re a great source of protein, iron and fibre, they’re much cheaper than meat and good for the climate.
3. Move more!
Being physically active is important to live a healthy life and it’s one of our Cancer Prevention Recommendations.
There’s also strong evidence that being active protects against cancers of the colon, breast and endometrium.
4. Eat more fibre
We should consume at least 30g of fibre a day. Eating a healthy balanced diet that contains plenty of fibre-rich food helps to support your general health and it helps to reduce your risk of bowel cancer.
5. Drink less alcohol
We have strong evidence to show consuming alcoholic drinks is a cause of 7 types of cancer and that there is no “safe” level of alcohol. Why not try a new mocktail recipe instead?
6. Eat more fruit
Fruit is a vital part of a healthy and balanced diet. It contains a variety of important vitamins, minerals and natural chemicals that our body needs.
7. Check your body regularly
Get into the habit of performing regular self-checks at home. As soon as you see or experience something new or something unusual, see a doctor. Even if it’s nothing, getting checked earlier is always better.
8. Eat more vegetables
Just like fruit (No6), it’s important to eat a range of vegetables. We have some evidence that eating non-starchy vegetables helps protects against some cancers of the mouth and throat.
9. Drink fewer fizzy or sugar-sweetened drinks
There’s strong evidence that regularly having sugar-sweetened drinks lead to weight gain over time, which can increase the risk of 13 types of cancer.
Stick to water or other unsweetened drinks, such as tea and coffee.
10. Eat less processed meat
There is strong evidence that consuming processed meat is a cause of bowel cancer. Ideally, you should cut back on all the bacon, sausages, pork pies and ham that you eat.
Research in 2023 showed that 8,500 bowel cancer deaths per year could be prevented if people stop eating processed meat.
11. Eat less red meat
Just like with processed meat, there’s evidence that too much red meat increases your risk of bowel cancer. But we don’t suggest you completely cut out red meat – it’s a good source of nutrients such as protein, iron, zinc and vitamin B12 so can form part of a healthy, balanced diet.
Our Recommendation is to eat no more than 3 servings of red meat a week. Opt for white meat and fish instead, or go meat-free.
12. Get better sleep
Sleep is vital for a healthy life, so whether it’s ditching screens before bed or establishing a routine, better sleep will have many benefits.
13. Opt for more wholegrains
Wholegrains are the seeds of cereal plants, such as wheat, barley, quinoa, oats, rye, maize (corn) and rice.
There’s evidence that they can decrease the risk of bowel cancer, as well as being a rich source of copper, zinc and dietary fibre.
14. Sign up to Activ8
If you’re looking to get more healthy – whether that’s increasing your activity levels, maintaining a healthy weight or eating better, why not join our FREE 8-week interactive programme?
It will be sent straight to your inbox 📧
15. Eat less fast food
There’s strong evidence that diets containing high amounts of “fast food” and processed foods high in fat, starches and sugars are a cause of weight gain, overweight and obesity, which has been linked to cancers.
A study in 2023 linked ultra-processed food to an increased risk of mouth and throat cancers.
16. Wear SPF and protect yourself from the sun
Each year, around 332,000 people are diagnosed with skin cancer globally, but a high-factor suncream, the right clothing and avoiding the sun between 11am–3pm can help decrease your risk.
17. Try a new recipe
Not only is it fun to cook new dishes, but it also introduces you to new flavours and can get you out of a rut of always cooking the same thing.
We have more than 350 healthy recipes to try – many of which are budget friendly, so you don’t have to break the bank.
18. Eat more protein
Protein is important for us maintaining our health and plays a role in maintaining your muscles, repairing any injuries, keeping your weight down (it keeps you fuller for longer), and it provides energy.
You don’t even need to eat lots of red meat to keep your levels up – nuts, seeds, eggs, wholegrains and pulses are all good sources of protein.
19. Get outside more
Keeping active is important and taking a break from screens and connecting with nature is good for both our mental and physical health.
Plus, spending 15 minutes a day in the sunshine helps restore the body’s vitamin D levels.
20. Ditch the sunbeds
If you want to get a tan, faking it is much safer.
21. Walk an extra 10 minutes a day
Get off the bus/train a stop early, or leave the car at home and walk to the shops. Small things add up quickly and soon you’ll prefer two legs over four wheels.
22. Sign up to our monthly newsletter
Get regular updates on our cancer prevention work, the latest research, health tips, new recipes and much more…
23. Have a meat free day
Or, why not try Veganuary? We’ve already mentioned that limiting red and processed meat is important for cutting your cancer risk.
And a 2022 study showed that following a vegetarian diet could cut your risk of cancer by 14%, so why not explore meat-free recipes.
24. Try a new sport or activity
If you’re in a slump or feeling generally demotivated, why not try something new? And, if sport isn’t your thing, gardening or yoga could get you moving more.
Alternatively, why not join a local group, such as a choir or a craft meet-up. Not only will you be learning something new, but you become part of a community, which provides multiple health benefits.
25. Change one thing
If this list has made you feel overwhelmed, don’t feel as you have to do them all. Start by picking just one thing to do differently and then build up from there. Before you know it, you’ll be thriving!

Sign up to hear more from us
We’ll bring health advice and tips, tasty recipes, the latest cancer research and much more direct to your inbox.
Science and football – while they may not seem like they have much in common, the disciplines meet in the person of Dr Frankie Brown. Frankie is an immunologist and former member of Scotland’s women’s team who has represented her country 96 times on the international stage.
Our funding helped Frankie realise her other dream of researching ways exercise can benefit those living with and beyond cancer.
Helping people with blood cancer

Frankie Brown with her Scotland team-mates
Under Dr Campbell from the University of Bath, Frankie worked in a team on a project funded by us investigating the effects of exercise on the health of patients with chronic lymphocytic leukaemia, a form of blood cancer that affects around 4,000 new people every year in the UK.
The team evaluated the safety and feasibility of a progressive exercise programme for these patients – many who were over 60. Essentially, they tested a “recipe for how to run a big study” more effectively, and even adapted it to continue successfully during the COVID pandemic.
She was inspired by her own background as a professional footballer, as well as her personal experience with cancer:
 “When I was finishing up my PhD, my mum died of breast cancer. That was a real trigger moment for me to look more into oncology. I just couldn’t get my head around it – she had been so healthy. I would wonder, what’s going on here?
“When I was finishing up my PhD, my mum died of breast cancer. That was a real trigger moment for me to look more into oncology. I just couldn’t get my head around it – she had been so healthy. I would wonder, what’s going on here?
“I already knew a lot about health and monitoring my body for football. I started playing football very young, playing with my little brother, and I haven’t stopped since. I was in the Scotland under 17s, then the under 19s, and got into the full squad when I was 21 and was there for 10 years.
“Having spent my whole life in a high-performance environment, with everything being tested and monitored, I became more aware of how my body reacts to even very small shifts in circumstances and situations. It wasn’t hard for me to see how those tiny changes that are so important to athletes can be important for everybody.”
This inspired Frankie to become a researcher, where she found herself on the team led by Dr Campbell and funded by us. There were, however, some setbacks along the way – the biggest being the COVID-19 pandemic. Thanks to the flexibility of our funding programme, Frankie says she and the rest of the team were able to pivot from designing the programme to be in-person, to buying the participants exercise bikes and running a group session over Zoom.
“We had to shift the whole design of the exercise sessions to be home-based and World Cancer Research Fund allowed us to deliver exercise bikes to the participants’ homes. Without that, the trial would have fallen apart.“
‘The more muscle mass you have as you get older, the more independent you will be’
The data showed a 2% increase in lean mass in the exercise group compared with a 0.4% decrease in the control group. This is a significant benefit, as Frankie explains: “The data we have now and the study we’ve done shows that any gain a patient can make with their performance can make a huge difference to their own wellbeing.
“An increase in lean mass – in other words, in muscle mass – in these patients is a huge thing, especially in people over 60. The more muscle mass you have as you get older the more independent you will be. One of our participants lived up some stairs, and whenever I think about the study, I think about them and hope that my work has made it easier for them to get the shopping up and down to their home.”
These results have informed the design of a larger study where Frankie and her team will assess the tumour-suppressing effects and mechanisms of exercise in humans.
Frankie is very vocal about the impact of our support on her work: “In my experience, World Cancer Research Fund has been incredibly supportive of me as a young academic. They’ve provided amazing flexibility at a very uncertain time. I wouldn’t have been able to achieve any of this without you.”
What do people who took part in the study say?
I was really unfit when I started the trial and in the battle with the bike I came near to collapse! But the research team were watching and got me sorted me out. So I didn't collapse and in fact went on to add 2kg to my muscle mass.
What do people who took part in the study say?
I’m pleased that I took part in the study as although I already did some exercise it pushed me out of my comfort zone and has left me feeling more positive about the future giving me a way to ‘fight back’.
A new study funded by World Cancer Research Fund has found that activity throughout the day, with peaks in the morning and late afternoon, correlated with an 11% reduced risk of developing colorectal (also known as bowel) cancer, compared with other patterns of exercise studied.
This study used accelerometer data (which measures movement) to analyse daily activity. It used a statistical method that examines all of the data and finds common patterns, and how those patterns might be related to the risk of colorectal cancer.
Researchers from Regensburg University utilised data from the UK Biobank, which had contacted 86,252 randomly selected individuals (56% of them women), asking them to wear accelerometers to track their movement over 1 week and following them for 5 years to monitor the development of colorectal cancer. When studying the data, researchers identified a 2-peak pattern of daily physical activity associated with reduced colorectal cancer risk.
The researchers identified 4 different patterns of physical activity throughout the day:
- Continuous day-long activity
- Activity later in the day
- Early and late-day activity
- Activity in the middle of the day and during the night
The 3rd pattern, where people were active both in the early and late parts of the day, was associated with an 11% lower risk of colorectal cancer, compared with 6% for day-long activity and no change for middle of the day and the night. Data from activity later in the day only was inconclusive. These findings held true even when considering factors such as smoking, shift work and other variables that could affect a person’s cancer risk.
Impact on sedentary lifestyles
In addition, the researchers found that a day-long activity pattern most effectively reduced colorectal cancer risk among individuals who were more sedentary. This may be because the effect of physical activity becomes more obvious when contrasted with a previously more inactive lifestyle, meaning that those who are fit and healthy are already at a reduced level of cancer risk. These findings show how beneficial physical activity can be, especially in those who are more sedentary.
Dr Helen Croker, Assistant Director of Research and Policy at World Cancer Research Fund, said:
“Being physically active is one of our Cancer Prevention Recommendations, and we know that this cuts cancer risk. These intriguing new findings offer potential for developing more specific recommendations, including patterns and timing of physical activity, for reducing cancer risk. This shows the vital importance of World Cancer Research Fund continuing to support research that expands our knowledge to inform cancer prevention going forwards.”
Prof Michael Leitzmann, Chair of the Department of Epidemiology and Preventive Medicine at the University of Regensburg, Germany, who was the lead investigator in the study, said:
“Our study highlights that not only is physical activity important for reducing colorectal cancer risk, but the timing of peak activity throughout the day could play a crucial role. By identifying specific times – early morning and late day – when physical activity is most beneficial, our findings open new avenues for targeted prevention strategies. If confirmed by future research, this could provide a simple yet impactful way for individuals to further reduce their cancer risk through the timing of their exercise.”
Read the paper
Stein, M.J., Baurecht, H., Bohmann, P. et al. Diurnal timing of physical activity and risk of colorectal cancer in the UK Biobank. BMC Med 22, 399 (2024).
About the UK Biobank
The UK Biobank is a large, population-based prospective study, established to allow detailed investigations of the genetic and non-genetic determinants of the diseases of middle and old age. It has 500,000 UK participants between the ages of 40–69.
About the University of Regensburg
The University of Regensburg is a nationally and internationally renowned comprehensive university with an excellent research spectrum, an attractive range of courses and a high sense of social responsibility. The UR stands for diversity, openness to the world and shaping the future. Its research strength is demonstrated by 6 Collaborative Research Centers funded by the German Research Foundation (DFG) and 9 grants from the European Research Council.
In 2017, the Institute for East and Southeast European Studies (IOS), an affiliated institute of the UR, was the first institution in Regensburg to be accepted into the renowned Leibniz Association, followed in 2022 by the Leibniz Institute for Immunotherapy, which emerged from the Regensburg Center for Interventional Immunology. In May 2024, the Regensburg Center for Ultrafast Nanoscopy opened at the university, where the ultra-fast quantum movements of atoms and molecules are researched using innovative, high-resolution slow-motion cameras. In spring 2022, the Science Council recommended funding for the Center for Immunomedicine in Transplantation and Oncology at the UR, a center for basic research in immunomedicine.
Dress right, rest right
It’s important to remember to dress appropriately for your workout and warm up just before, especially if you’re exercising outside. Shoes with good grip, warm clothes, gloves, a headband or beanie, and a scarf or snood can help you avoid getting too cold, sick or injured. And don’t forget to rest and recover, including stretching after.
Keeping active in winter may have its challenges, but setting SMART goals and creating a routine to build healthy habits can help you achieve your goals. Embrace the chill, stay active and watch it transform your overall well-being during the winter season and beyond!
Are you interested in building healthy habits? Sign up to Activ8, our free 8-week online behaviour change programme that can help you achieve your health goals, including being more active.