The UK government published its 10-year Health Plan on 3 July, setting out its ambitions to reform the health system and shift the focus from sickness to prevention.
As a cancer prevention charity with a vision of a world where no one dies from a preventable cancer, we welcome the Plan’s direction but there are many key areas of health policy where it simply falls short of what the public needs.
Positive inclusions
Many of the commitments in the Plan had already been announced and were warmly received, such as the expansions of free school meals and the Soft Drinks Industry Levy.
Encouragingly, the Plan also includes new mandatory measures that mark a meaningful step towards creating healthier environments for all.
These include:
- Mandatory healthy food sales reporting for all large companies in the food sector.
- Mandatory healthy food standard to improve the healthiness of sales.
- Updates to the nutrient profile model, used to set marketing restrictions on junk food.
- 10% uplift to restore the value of the Healthy Start scheme from 2026–27.
- Mandatory labelling on alcoholic drinks to include consistent nutritional information and health warning messages.
- Place-based approach to physical activity, including £250m for 100 places via Sport England, at least £400m for local community sports facilities, and new school sport partnerships.
- National walking and running campaign led by Sir Brendan Foster.
- Development of a new physical activity strategy.
These measures are welcome steps forward in improving our food and drink environment and enabling people to be more physically active.
We hope the forthcoming National Food Strategy will drive deeper systemic changes to ensure affordable, accessible healthy food for everyone in England.
Critical missed opportunities
On alcohol, the Plan falls short of prioritising the range of evidence-based policies proven to reduce alcohol consumption, which causes around 17,000 UK cancer diagnoses each year.
Notably, it fails to include minimum unit pricing (MUP) for alcohol in England, despite the success of MUP in reducing alcohol-related deaths in Scotland and Wales. Worryingly, England continues to lag the devolved nations on this crucial policy.
The Plan also makes no mention of strengthening marketing restrictions on alcohol, and so enables industry to continue to normalise drinking as an aspirational lifestyle choice.
Given the rising number of alcohol-related deaths each year, we are urging the UK government to deliver a National Alcohol Strategy for England. As outlined in our recent letter to the Prime Minister, Keir Starmer, during Cancer Prevention Action Week, we continue to call for bold action on alcohol-related cancer.
Equally disappointing is the absence of action to strengthen protections and support for breastfeeding and infant feeding. There are no new mandatory, independently enforced regulations on the composition, marketing and labelling of baby and toddler foods. This is a missed opportunity, particularly in light of the UK government’s stated goal to raise the healthiest generation of children ever.
We will continue to urge the government to adopt the recommendations of the Competition and Markets Authority’s market study on infant and follow-on formula.
Turning ambitions into action
This Plan arrives as Labour marks its first year in government under Starmer. This government now has the opportunity – and responsibility – to turn its prevention agenda into lasting structural change that improves the nation’s health.
The upcoming National Cancer Plan for England presents a further chance to address modifiable risk factors and fill the gaps left by the 10-year Health Plan.
We welcome the Prime Minister’s willingness to challenge accusations of “nanny statism” and urge the government to ensure all health strategies are protected from undue industry influence.
We want prevention to be the foundation of all health strategies. We stand ready to bring our scientific and policy expertise to the table – and we’re calling on the UK government to work with us to turn bold ambition into real change, helping millions live longer, cancer-free lives.
In our resource library
Further reading
Key takeaways:
- The CO21 CHALLENGE Trial found that a structured exercise programme after chemotherapy led to a 28% lower risk of cancer recurrence in colon cancer survivors compared with usual care.
- This is the first randomised controlled trial (RCT) to show that exercise directly improves survival in colon cancer patients. It confirms what observational studies have long suggested.
- The results were presented at a recent conference and made headline news. Experts say the CHALLENGE Trial marks a shift from viewing exercise as a “nice to have” to a “need to have” in cancer care.
Colon (part of the large bowel) cancer survivors who took part in a 3-year structured exercise programme had a 28% lower risk of cancer recurrence or a 2nd cancer. They also had a 37% lower risk of death compared with usual care.
These findings were shared at the 2025 Association of Clinical Oncology (ASCO) Annual Meeting. They were also published in the New England Journal of Medicine.
The ASCO Annual Meeting is the world’s largest oncology conference. It attracts more than 40,000 attendees from around the world. Every year, ASCO highlights the latest advancement in treatments. It also shares the directions that have the greatest potential for progress and patient impact.
Spotlight on exercise
The CO21 CHALLENGE Trial pulled back the curtain on a weapon that has been hiding in plain sight: physical activity. The results of the trial showed improvement in disease-free survival and overall survival in colon cancer survivors in the aerobic exercise intervention group. This trial is the first gold standard RCT to show what has long been indicated from observational studies. This is a big deal!
The impact of exercise on cancer outcomes has been a topic of great debate. Observational research has shown improvements in survival and quality of life linked to higher levels of physical activity. However, observational study designs are limited. They do not show cause and effect.
Plus, they are hard to implement in clinical settings due to concerns that the reported effects may not truly reflect the impact of exercise (and may be due to something else).
Our research
Over the past few years, World Cancer Research Fund International has done extensive reviews through its flagship Global Cancer Update Programme (CUP Global).
CUP Global includes partnerships with American Institute for Cancer Research, World Cancer Research Fund in the UK and Wereld Kanker Onderzoek Fonds in the Netherlands.
Our CUP Global reviews look at the extent to which diet, nutrition and physical activity impact people after a diagnosis of breast and colorectal cancers with regard to:
- cancer-specific mortality
- all-cause mortality
- risk of cancer recurrence
- health-related quality of life
An expert panel judged the strength of this CUP Global evidence. There were some limitations. Still, detailed recommendations were made to strengthen future research. One of the key recommendations was for well-conducted trials to look at the impact of nutrition or physical activity. The CHALLENGE trial is therefore very timely.
The CUP Global analysis was published in the International Journal of Cancer. It was cited several times in the CHALLENGE trial manuscript.
The CUP Global analysis compared highest with lowest levels of activity. We found that all-cause mortality was reduced by 23–40% depending on physical activity exposure.
Prof Anne May, University Medical Centre, Utrecht
During our review of the literature concerning the impact of post-diagnosis physical activity on colorectal cancer prognosis for the Global Cancer Update Programme (CUP Global), we were unable to draw strong conclusions due to lacking evidence from randomized controlled trials. The Challenge trial provides exactly the evidence we were waiting for.
The summary estimate for studies that assessed activity dose was measured in MET hours per week.
- A 10 MET hour per week increase in activity was linked to a 24% reduction in all-cause mortality.
- A change of 10 MET hours per week was also the intervention goal in the CHALLENGE trial.
The effect sizes in this first, gold-standard RCT are remarkably well-aligned with the CUP Global analyses of observational studies.
During the presentation of the trial results at ASCO, the authors shared this chart. It includes the treatment benefits from approved therapies for colon, lung and breast cancer.
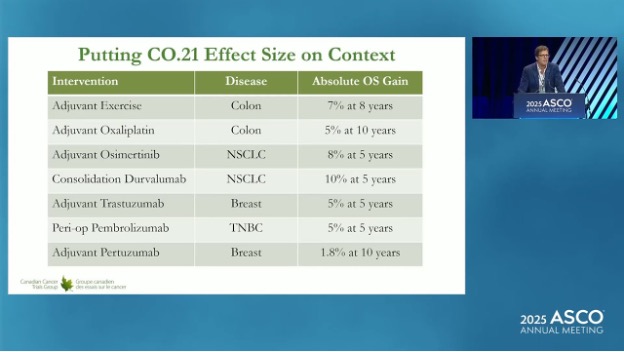
With 7–8% gains, you can see that exercise compares very favourably with other approved therapies in terms of absolute overall survival gain.
Collecting clinical trial evidence
The CHALLENGE trial confirms the clinical benefits that had been reported from observational studies. However, previous RCTs have also hinted at the accuracy of the results from observational studies. For example:
- The LEANer trial was published in 2023. It showed that triple negative breast cancer patients randomised to a diet and physical activity intervention before chemotherapy had a 53% higher rate of treatment success (eliminated cancer cells).
- A trial published in June 2025 showed that an exercise programme during and after chemotherapy increased the immune system responses in oesophageal cancer patients.
World Cancer Research Fund will fund the Optimus trial in the UK. Dr David Bartlett and Prof Adam Frampton at the University of Surrey will lead this study. It was proposed due to these findings.
Next steps
Dr Kerry Courneya co-led the CHALLENGE trial. At ASCO, he said these results could change practice for high-risk stage 2 and stage 3 colon cancer.
He expressed reservation that these results could be generalised to other sites and cancer stages. But he was optimistic that similar trials could be done more quickly than the CHALLENGE trial by taking advantage of newer methods. This could include using remote exercise assessments or activity trackers.
Dr Courneya noted that “support from funding agencies like WCRF/AICR is critical to moving this field forward because of limited access to funding for lifestyle research”.
AICR recently funded a project linked to the CHALLENGE Trial. It is led by Dr Kristin Campbell at the University of British Columbia in Canada. It will look at how muscle and fat tissue respond to exercise and how that may contribute to the observed survival benefits.
The response to the CHALLENGE Trial has made media headlines. Cancer researchers, doctors and patients are also excited by the news. This suggests that adding exercise as an additional part of treatment will gain further momentum.
While more trial data will be needed to support broader implementation, we are likely leaving the “nice to have” approach to exercise oncology and entering the “need to have” phase!
Research grants on physical activity
A selection of some of the grants we have funded that focus on the impact of physical activity on people living with and beyond a cancer diagnosis.
We’re excited to announce that World Cancer Research Fund has joined Our Future Health, the UK’s largest health research programme, as an affiliate partner.
With cancer rates rising and modifiable factors contributing to around 40% of all cases, the partnership represents a bold step in harnessing large-scale health data and decades of scientific insight to prevent more cancers before they start.
The UK Director at World Cancer Research Fund, Steven Greenberg, said:
“It’s tremendously exciting to be a part of the UK’s largest, most diverse health research programme. We know that 40% of cancers can be prevented through modifiable factors such as diet and exercise. With a growing rate of diagnoses, collaboration to better understand these risks is more important and timelier than ever.
“By working together, we’ll be able to combine our own extensive knowledge and experience on cancer prevention with the knowledge and insight coming from Our Future Health to further understand how cancer risk can be affected by diet and lifestyle.
As an affiliate partner, we’ll contribute our global expertise in the links between diet, weight, physical activity and cancer risk, helping guide Our Future Health’s work in identifying preventable risk factors. In turn, we’ll benefit from collaborating with the UK’s largest health research programme – enabling new insights into early detection and public health strategies.”
About Our Future Health
Our Future Health is the UK’s largest ever health research programme. It is designed to help people live healthier lives for longer through the discovery and testing of more effective approaches to prevention, earlier detection and treatment of diseases. Our Future Health is inviting millions of people, from all backgrounds and from across the UK, to take part. Volunteers are providing information about their health and lifestyles to create an incredibly detailed picture that represents the whole of the UK.
Dr Raghib Ali, CEO and Chief Medical Officer of Our Future Health, said:
“We’re so pleased to welcome World Cancer Research Fund as our newest affiliate charity partner. We know that cancer will affect half of us in our lifetimes, and together we want to improve cancer prevention, so more people can live longer, healthier lives. Their expertise in funding life-saving research will be really valuable for Our Future Health.”
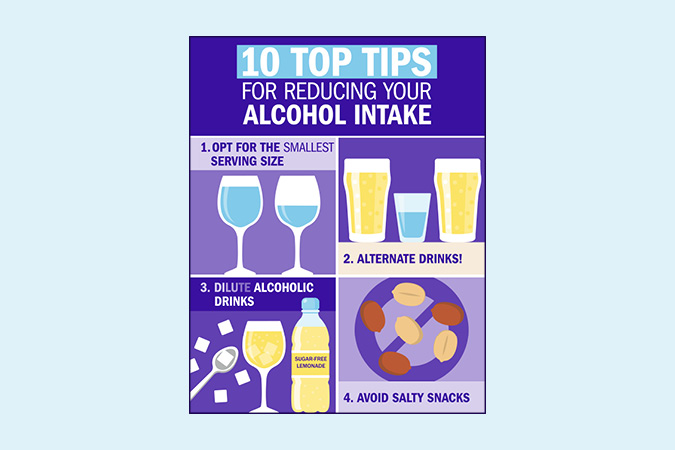
To celebrate Cancer Prevention Action Week and to kickstart summer, we’ve pulled together our favourite mocktail and alcohol-free drink recipes, which are perfect for events from parties to BBQs, day or evening.
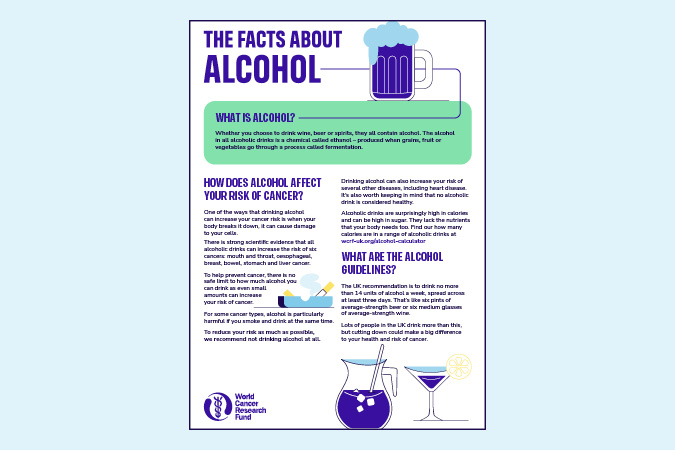
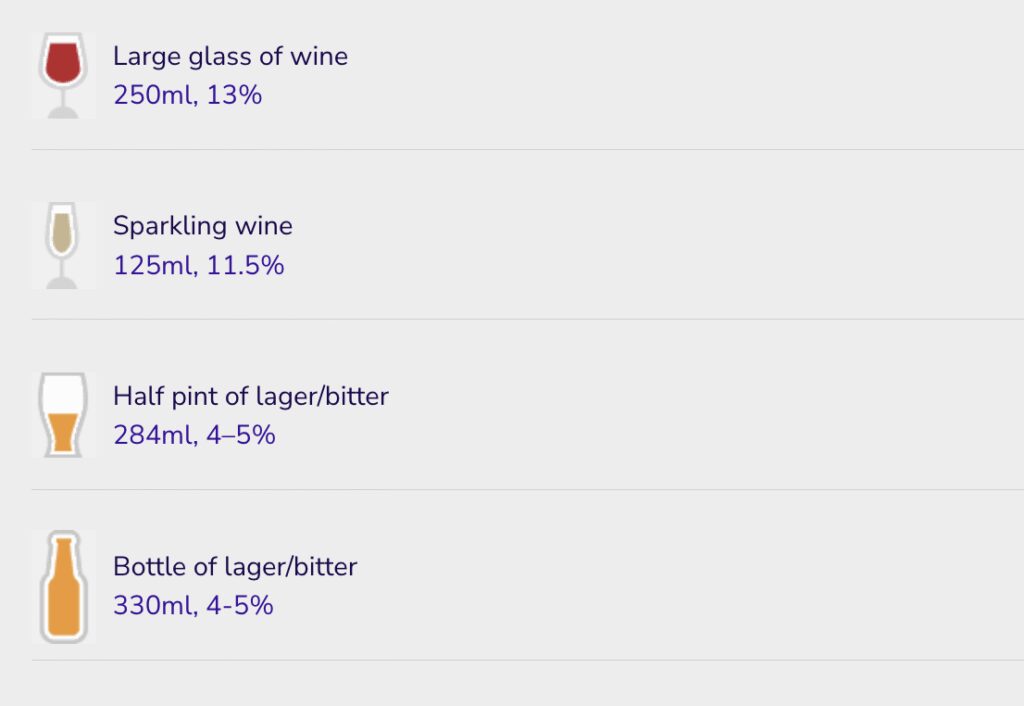
Did you know that drinking alcohol increases your risk of 7 types of cancer, including breast and bowel?
Alcoholic drink can also have a lot of hidden calories. Reducing how much alcohol you drink may support weight management, which in turn can help lower your risk of cancer. Unlike many alcohol-free drinks you find in a shop or pub, our mocktail recipes are all lower in calories with no added sugar.
Our top 7

Alcohol-free G&T
Enjoy the crisp tones in our no-alcohol gin and tonic, with a grapefruit twist for something different this summer.
⏰ 5 minutes
🍎 1 of 5 A DAY
🧍♂️ serves 2
 Berry sparkle
Berry sparkle
For a healthy alternative to prosecco, our refreshing berry fizz is a perfect option, and so easy to make.
⏰ 5 minutes
🧍♂️ serves 2

Pink lemonade
A family favourite, our rose-blueberry lemonade is a great addition to any BBQ.
⏰ 5 minutes
🧍♂️ serves 2
 Watermelon slushie
Watermelon slushie
Enjoy the tangy notes of watermelon, raspberries and lime with this healthy slushie.
⏰ 10 minutes
🍎 1 of 5 A DAY
🧍♂️ serves 2
 Peach iced tea
Peach iced tea
In warmer weather, a hot cup of a tea isn’t always the best, so this peach iced tea is a refreshing alternative to enjoy during the summer months.
⏰ 10 minutes plus cooling
🍎 Less than 1 of 5 A DAY
🧍♂️ serves 8
 Cucumber cooler
Cucumber cooler
Refresh yourself on dry days with a summery cucumber cooler that kids will love.
⏰ 5 minutes
🧍♂️ Serves 2
> Get the recipe
On the blog
As part of Cancer Prevention Action Week 2025, on Wednesday we handed in an open letter and petition, alongside breast cancer survivors Dr Liz O’Riordan and Nikki Bednall, and the Alcohol Health Alliance.
The letter (below) – signed by more than 25 organisations and health experts – and the petition called on Prime Minister Sir Keir Starmer and his government to introduce a National Alcohol Strategy to Prevent Cancer, as part of our Cancer Prevention Action Week (CPAW) activity.
This year, CPAW is highlighting the links between alcohol and cancer – our research shows that most people don’t know that drinking any amount of alcohol increases the risk of 7 types of cancer.
What’s more, around 17,000 new cases every year are down to alcohol – so we’re urging the UK government to introduce a long-overdue National Alcohol Strategy for England – one that tackles alcohol harm head-on through:
- mandatory health warnings highlighting cancer risk
- minimum unit pricing
- marketing restrictions
to reduce consumption, lower cancer risk, and protect lives.





Read the full letter below
The Rt Hon Keir Starmer MP
Prime Minister
10 Downing Street
London SW1A 2AA
CC: The Rt Hon Wes Streeting MP, Secretary of State for Health and Social Care
Ashley Dalton MP, Parliamentary Under-Secretary of State for Public Health and Prevention
25 June 2025
The UK government must act on alcohol now to prevent cancer
Dear Prime Minister,
On behalf of more than 20 organisations and public health leaders, we are writing to share our deep concern about the continued lack of action to reduce alcohol consumption across the United Kingdom. In particular, the absence of a National Alcohol Strategy for England stands in stark contrast to the scale of harm caused by alcohol, with alcohol-specific deaths having increased by 42% in England between 2019 and 2023 alone.
This week marks Cancer Prevention Action Week (CPAW) – a national campaign led by World Cancer Research Fund (WCRF) – which seeks to empower the public and inspire change to prevent cancer. This year, CPAW is shining a spotlight on the link between alcohol and cancer, and the urgent need for government action.
In the UK, alcohol causes around 17,000 cases of cancer every year – equivalent to 46 people receiving a diagnosis every single day. And as our population ages and grows, these numbers are projected to rise. Worryingly, the pandemic has also driven an increase in high-risk drinking. Modelling by the Institute of Alcohol Studies and Health Lumen suggests that if this trend persists, we could see an additional 18,785 cancer cases by 2035.
Public awareness remains alarmingly low that alcohol is a Group 1 carcinogen, the same category as tobacco and asbestos, and a cause of seven types of cancer, including two of the most common breast and bowel as well as mouth and throat, oesophageal, liver and stomach cancer. These risks are present even at low levels of consumption. New polling commissioned by WCRF reveals that when asked unprompted only 1 in 14 UK adults are aware that alcohol increases cancer risk and 25% believe there is no health risk attached to drinking alcohol.
We are not alone in our concern – thousands of members of the public including more than 20 organisations have signed our petition calling for greater government action. They agree that no one should have to suffer the devastating trauma of alcohol-related cancer.
The human toll is compounded by the economic burden. In 2016, Cancer Research UK estimated that alcohol-attributed cancers cost the NHS alone an estimated £100 million annually. With the health service under immense strain, it is imperative to act now and realise the government’s priority of prevention.
Despite alcohol being the sixth leading cause of preventable cancer in the UK, current policy does not reflect this reality. We urge the government to fulfil its responsibility to protect public health by introducing a National Alcohol Strategy for England without delay, which must include:
- Mandatory alcohol product labelling with health warnings, including information on cancer risks and calorie content.
- Marketing restrictions on alcohol by classifying it as an ‘unhealthy product’ under high fat, salt and sugar marketing restrictions.
- Implementing and evaluating minimum unit pricing at 65p in England with rates adjusted in line with inflation, to bring England into line with Scotland, Wales and Northern Ireland who all either have MUP already or have stated their intention to implement.
It is vital that this strategy aligns with the forthcoming National Cancer Plan for England, ensuring that alcohol is comprehensively addressed as a modifiable risk factor for cancer. We also urge the UK government to work in close collaboration with the devolved administrations, particularly to enable action to improve approaches to labelling and advertising. All policy development processes must be protected from industry influence and vested interests to ensure public health is placed above profit.
Such action would not only help to reduce cancer risks but reduce other alcohol-related harms. It would also support the government’s own ambitions to shift from sickness to prevention, as set out in the Health Mission, and contribute to economic growth by reducing illness-related inactivity.
We stand ready to support this effort and urge you to act now. Together we can tackle the devastating impact of both alcohol harm and cancer.
Yours sincerely,
Rachael Gormley, Chief Executive, World Cancer Research Fund
Dr Richard Piper, CEO, Alcohol Change UK
Alison Douglas, Chief Executive, Alcohol Focus Scotland
Professor Sir Ian Gilmore, Chair, Alcohol Health Alliance
Greg Fell, President, Association of Directors of Public Health
Dr Heather Grimbaldeston, Chair, BMA Public Health Medicine Committee, British Medical Association
Professor David Strain, Chair, BMA Board of Science, British Medical Association
Thalie Martini, Chief Executive Officer, Breast Cancer UK
Eddie Crouch, Chair, British Dental Association
Pamela Healy OBE, Chief Executive, British Liver Trust
Jill Clark, Chair, CancerWatch
Alison Wise, Communications Manager, on behalf of Fight Bladder Cancer
Ailsa Rutter OBE, Director, Fresh and Balance
Kostas Tsilidis, Associate Professor of Cancer Epidemiology and Prevention, Imperial College London
Dr Katherine Severi, Chief Executive, Institute of Alcohol Studies
Dr Dominique Florin, Medical Director, Medical Council on Alcohol
Daniela Binnington Nessman, Founder, Menopause and Cancer
Gopika Chandratheva, Nutritionist, NHS
Tamara Khan, CEO, Oracle Head & Neck Cancer UK
Jon Coleman-Reed, Head of Operations, Prevent Breast Cancer
Dr Claire Shannon, President, Royal College of Anaesthetists
Robert Steele, Chair, Board Directors, Scottish Cancer Foundation
Dr Alastair MacGilchrist, Chair, Scottish Health Action on Alcohol Problems
Chris Curtis, Chief Executive Officer, Swallows Head & Neck Cancer Support Charity
Amandine Garde, Professor of Law & Non-Communicable Diseases Research Unit, University of Liverpool
Richard Cooke, Professor of Health Psychology, University of Staffordshire
Dr Kathryn Scott, Chief Executive, Yorkshire Cancer Research
‘Who Comes Here?’, ‘A Grenadier’ – Victorian nursery rhyme illustration (Getty Images). From “Nursery Rhymes – Ridicula Rediviva” illustrated by J.E. Rogers, with chromolith printing by R. Clay Sons & Taylor and published in London in 1876 by Macmillan and Co.
World Cancer Research Fund has been highlighting the links between alcohol and cancer for more than 30 years – but we weren’t the first to do this.
In fact, as Britain recovered after the First World War, beer producers launched campaigns to get people – especially men and boys – back into the pub, with slogans such as “Guinness is good for you” and “Beer is best”. Yet this move by beer makers was a reaction to the thriving temperance movement, which fought back with postcards that said: “Beer is best – for cancer”, listing the cancers alcohol was associated with including brain and mouth.
This is just one aspect of the long history of drinking – and sobriety – in Britain. Did people really drink beer because water was unsafe? Why did people turn to gin? And was Irn-Bru an original tipple of choice for teetotallers? Read on to find out.
Small beer gets bigger
We know through archaeological deposits that people have been drinking beer for around 13,000 years. Beer has certainly been an important drink – especially for poorer people – in the UK for more than 1,000 years. In the Medieval era (around 5th–15th centuries), beer was not just a staple drink. It was also a vital source of calories. At that time, beer and ale were graded according to how long the liquid had been fermented, its strength and the quality of the ingredients. “Small beer” was the weakest and most widely drunk option. Prof Phil Withington of the University of Sheffield says: “Small beer was an integral feature of British diets and was drunk at all times of the day from breakfast.”

A man dressed up as a medieval monk pours himself some beer. Getty Images
However, it’s not true that everyone had to drink beer because the water was unsafe. Most people at this time would have lived in rural areas, and local rivers and streams would have been a source of drinking water. Both beer and ale were safer than some water sources, though, because they are heated during production.
A major change in Britain’s drinking habits occurred in the 1700s onwards with the arrival of gin – dead cheap and often home brewed – which coincided with the start of the industrial revolution, when people moved on mass from rural, family dwellings to less sanitary urban and suburban areas. The pub became a respite for people after working long hours in factories and provided an escape from cramped multi-generational living conditions. “Drink was everywhere; it was economically important and culturally unavoidable,” Dr David Beckingham told History Extra.
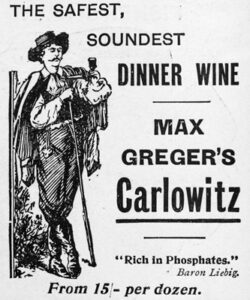
Antique advertisement from British magazine: Dinner wine
Gin sends Britain wild
Gin was widely available, low-taxed and – incredibly – sold in pints as people were accustomed to drinking beer in pints. Gin is distilled rather than fermented – which means it’s a lot stronger. Stories we’re familiar with today – around binge drinking, the social impact of alcohol harm (especially when women and poorer people drink to excess), and attempts to curb drinking through public pressure, moral panics and legislation – all began with the Gin Craze. Then as now, alcohol had a class element, with the wine and champagne drunk by the rich seen as less damaging to society and health than the beer and gin of the poor.
And today’s sober curious movement has its history in the anti-drink movements that started at this time. Initially, the backlash against gin focused on temperance – encouraging people to limit their alcohol consumption, mainly by drinking weaker but still alcoholic drinks. The 1830 Beerhouse Act allowed people to brew beer from home – an attempt to reduce gin drinking. However, some strands of the movement favoured total abstinence.
The Band of Hope, established in 1847, became the biggest temperance organisation in Britain, with 3.5 million members by the end of the 19th century. It was a youth-led movement, and part of the attraction was that it offered young people an (often cheaper) alternative to the pub. As well as pressurising members with signed pledges, badges and magazines, temperance societies organised fun stuff: brass bands, sober cafes, music hall events and outings. The first temperance day trip was an excursion from Leicester to Loughborough in 1841, for 500 temperance society members. The man who arranged it was none other than Thomas Cook – the inventor of package holidays.
So what alcohol-free drinks were around in the 18th and 19th centuries? Initially, most concoctions were mixes of readily available herbs and water, often heavily sweetened: sarsaparilla “wine”, dandelion and burdock, cream soda and ginger beer – as well as tea. Some of the biggest brands in soft drinks also emerged at this time. Teetotallers drank fortifying iron brew (later Irn Bru), Coca-Cola and Vim Tonic, as well as milk drinks – precursors of today’s milkshake and bubble tea bars.
It wasn’t plain sailing for those trying to cut back on alcohol though. The temptations of alcohol versus the guilt of overindulgence are revealed in the diaries (written between 1830 and 1881) of Nottingham solicitor and mayor William Parsons, who talks about his attempts to go dry in January, and how hard it was to avoid booze in social gatherings: “Tea totalism in my position is not carried out without great difficulty.”
As well as persuading individuals to change their drinking habits, people who advocated for drink-free living leaned on politicians to legislate for restrictions on the sale of alcohol, and taxation to reduce its availability and affordability. The fact that we’re trying the same approaches hundreds of years later shows the difficulty of breaking up Britain’s relationship with the booze.
Temperance as a movement died off from the 1950s as alcohol became even more widely marketed and socially acceptable. This is perhaps reflected in the licensing changes. Since 1988, pubs have been able to open all day and 24-hour licensing was introduced in 2005. Despite this, younger generations seem to be drinking less than their elders. In England’s 2022 health survey, the highest prevalence of drinking on at least 1 day a week was among adults aged 65–74, whereas the lowest was among 16–24-year-olds (60% vs 36%).
Our theme for Cancer Prevention Action Week is Alcohol and cancer: let’s talk. The UK’s long history of drinking – and staying sober – shows that alcohol is deeply embedded in British society. Yet even though we’re no longer in the midst of a gin craze, the harms of alcohol are widespread. As those abstinence campaigners at the start of the last century knew, alcohol is a cancer-causing, psychoactive, toxic, and dependence-producing substance linked to more than 200 health conditions. Everyone deserves to know the history – and the truth – about alcohol.

Prof Richard Cooke
Prof Richard Cooke is interested in what motivates people to drink alcohol – he surveys people to find out how psychological variables such as the intention to drink, attitudes about drinking, and regret after drinking alcohol – can predict how much people consume.
“Most of my research has been done with young adults aged 18–30,” says Prof Cooke, “because they were traditionally seen as the group that drinks the most, but this has changed in the last decade. I’m now doing much more research with middle-aged people. I also do studies assessing awareness of drinking guidelines, comparing how young adults and policymakers talk about alcohol, and reviewing the effectiveness of alcohol interventions.”
‘We know it’s dangerous’
“I find alcohol consumption fascinating to study as drinking has high social approval even though we know it’s dangerous. This means that health messages about alcohol are trickier to create than smoking messages. Saying ‘Don’t smoke’ is quite acceptable; saying ‘Don’t drink alcohol’ is less so,” he says.
Prof Cooke has several theories about why alcohol remains so popular across cultures: “Alcohol is a social lubricant: it relaxes people, makes them feel more confident and more able to socialise, especially with strangers. It’s really tied to our psychology in many different, sometimes unexpected, ways.”
A former student of Prof Cooke, Dr Joel Crawford, did his doctorate degree on regret and drinking. He asked young people adults about the fear of missing out (Fomo). When they don’t drink, some people think they are missing out on an enjoyable experience, like missing a party because you have to work. Dr Crawford found that the young adults would rather experience alcohol harms, such as hangovers and feeling sick, than miss events that heavily included alcohol, saying “Fomo was more painful to them than a hangover!”
This study illustrates the social and emotional barriers people trying to drink less may encounter. “It’s the social acceptability of drinking in most situations that makes it a challenge to reduce; drinking is associated with celebrations – birthdays, weddings, getting a new job, becoming a parent– and commiserations – missing out on promotion or the death of a loved one. Alcohol is also linked to healthy activities, like ending a walk in the countryside with a drink in a pub.”
Drinking’s a habit

“At the individual level, drinking habits are an issue. People develop habits when they perform the same behaviour in a stable setting, like drinking every Friday night in the pub with your friends. Breaking this habit means unpicking your routines in ways that people often don’t want to do.”
However, based on current trends, there will be fewer people drinking into middle-age and later life: “This has the potential to dramatically change how we organise events,” says Prof Cooke, comparing it to the rise in the availability and acceptability of non-dairy alternatives to milk. “People will be asking for non-alcoholic drinks at parties, and maybe that will become as acceptable as asking for an alcoholic drink is now.”
Young people prefer to stay in control
We asked Prof Cooke about why there is a decline in young people drinking alcohol. “There are several theories about why this is happening. One is that young people spend a lot of time online, and they want to present the best possible version of themselves as someone who is in control. Studies of Facebook content show that people generally share positive alcohol content, rather than negative experiences.
“Another idea is that alcohol has become more expensive in the last decade or so, which has put young people off drinking. Finally, the rise of energy drinks may be part of the explanation too, especially for young people who like to play games online. Energy drinks, high in caffeine, are likely to aid video game performance. Alcohol is unlikely to do this.”
For people of any age trying to limit their alcohol, Prof Cooke recommends trying to understand the reasons why you drink. “Do you drink to be sociable, to enhance an evening out, to cope with negative emotions? Are there other ways you could meet those needs? Psychological interventions, such as feedback on drinking or setting goals to drink less, can also be effective ways to cut back.”
Prof Cooke’s latest research
Prof Cooke’s latest research is published in Drug and Alcohol Review. He says: “Our new paper shows that policymakers and drinkers talk about drinking in different ways. While policymakers focused on drinking behaviour, drinkers talked about how drinking made them feel different emotions: embarrassed, happy, guilty, sad. Policymakers need to construct policies to reflect the importance of emotions in drinkers’ narratives.”
> Read the paper: The language of alcohol: Similarities and differences in how drinkers and policymakers frame alcohol consumption
Alcohol and cancer: let’s talk
In the UK, alcohol is a major part of how many of us socialise, relax, and celebrate. But do we really know the risks we’re taking when we drink?
Our research shows that most people don’t know that drinking any amount of alcohol increases the risk of 7 types of cancer.
This Cancer Prevention Action Week, we want to spark a national conversation: with friends, family – and within government – about alcohol and cancer.
Cancer Prevention Action Week
This year’s campaign focuses on the links between alcohol and cancer.
You’re socialising with friends. Someone asks what you want. You say: “Oh – I’m not drinking tonight.” And then comes the follow-up:
- Why not?
- Are you on antibiotics?
- Are you pregnant?
- Are you ill?
- Just have one. Come on, it’s Friday.
It’s a scene that plays out thousands of times every weekend in the UK. For a choice that should be straightforward – not having an alcoholic drink – we’ve made it weirdly taboo.
But people say “no thanks” to alcohol for all kinds of reasons.
- They’re trying to sleep better
- They’re dealing with anxiety or illness
- They’re thinking about fertility
- They’ve had a rough week and can’t face a hangover
- They’re training for something
- Or they’re just… not in the mood
And yet that simple choice often triggers awkwardness, suspicion – even ridicule. Why?
Alcohol has become a shortcut for belonging or fear of missing out
So many of us drink to connect, to relax, to mark the end of the day. And saying ‘no’ interrupts that flow. It disrupts the unspoken script: “We’re all doing this together”.
But when choosing not to drink becomes a social problem, we have to ask:
Why is drinking so protected? What are we not talking about?
That’s why – as part of Cancer Prevention Action Week 2025 – we want to get people talking.
‘No thanks’ shouldn’t need a justification
Imagine if we stopped asking people why they’re not drinking – and started asking how can we make not drinking more comfortable for everyone?
Or how can we support them in their choice?
You shouldn’t need to have a serious illness, or be training for a marathon, or whisper that you’re trying for a baby to opt out of alcohol.
And yet, we’ve made not drinking feel like a confession.
This isn’t about demonising alcohol. It’s about giving people the facts and allowing them the space to make different choices – for any reason, or for no reason at all.
Alcohol and cancer: the facts
Alcohol is a Group 1 carcinogen – that means it can cause cancer – putting it in the same category as asbestos, tobacco and plutonium.
Alcohol is directly linked to 7 types of cancer, including:
- Breast
- Bowel
- Liver
- Mouth and throat
- Oesophagus
- Stomach
Even small amounts increase your risk. For example, just 1 drink a day raises your breast cancer risk by around 7–10%. For bowel cancer, the risk starts rising even at low levels of drinking.
But while this science has been clear for years, our polling revealed that 1 in 4 of us don’t associate any health risks with alcohol.
We’re not being given the information we need to make informed choices – and when people do make those choices, they often feel judged, questioned or excluded. That’s wrong.
How do we shift the culture?
1. We normalise ‘No’
We make not drinking visible, valid and unremarkable. The more people hear “No thanks” without a 5-minute explanation, the more normal it becomes.
2. We get curious, not confrontational
When someone doesn’t drink, it’s not a rejection of you – it’s a choice for them. We stop taking it personally. And offer support.
3. We name the stakes
This isn’t just about social awkwardness. It’s about informed choice and health. The cancer link is real, as are the 200 other health conditions associated with alcohol. People deserve to know – and not be made to feel odd when they act on it.
If you’re doing other things to live well – eating healthily, counting your steps, trying to sleep enough – why should people be made to feel awkward about not drinking alcohol?
Ready to change the conversation? Read to say “No thanks”?
Only 16% of us in the UK feel at ease discussing our relationship with alcohol, ranking it among the least talked about topics – less so than sex (17%) and money (29%), according to our poll.
We’re emphasising the connection between alcohol and cancer as part of Cancer Prevention Action Week, which starts today. We have strong evidence that alcohol increases the risk of 7 cancers:
- Breast
- Bowel
- Head and neck
- Oesophageal
- Liver
- Stomach
Alcoholic drinks are also high in calories and often high in sugar, increasing the risk of gaining weight. Living with overweight or obesity increases the risk of at least 13 types of cancer.
We surveyed 2,000 people to gain insights into Britain’s understanding of alcohol and cancer risks. The findings reveal consistent misconceptions regarding alcohol’s dangers. Alarmingly, 25% of respondents did not associate any health risks with alcohol, and only 1 in 14 mentioned cancers as a risk when asked unprompted.
These misconceptions may hinder our ability to have informed conversations about alcohol. About 4% of cancer cases in the UK are attributed to alcohol, meaning that, each year, around 17,000 people are diagnosed with cancer caused by alcohol. Adding to this immeasurable human cost is the economic burden. Alcohol-related cancers cost the NHS around £100m every year.
We need a National Alcohol Strategy
We support clearer public health messaging to raise awareness of the real dangers of alcohol consumption, as well as other measures such as health warning labels. Alongside many other health organisations in the UK, we’re urging the Prime Minister, Sir Keir Starmer, to implement a National Alcohol Strategy for England.
World Cancer Research Fund CEO Rachael Gormley
Alcohol is pervasive in our lives, from celebrations to after-work drinks. But do we truly understand the risks involved? It’s essential that we engage in more discussions about alcohol and cancer, empowering individuals to make informed health choices.
Alcohol Health Alliance Chair Sir Ian Gilmore
One of the reasons public awareness is so low is that we're being kept in the dark about the true cost of drinking. People have the right to know the full picture so that they can make informed choices about what they consume.
World Cancer Research Fund Executive Director of Research and Policy Dr Giota Mitrou
A long-overdue National Alcohol Strategy in England would help the government tackle alcohol harm head on – reducing consumption, lowering cancer risk, and protecting lives.
Nikki Bednall is a World Cancer Research Fund Supporter and breast cancer survivor. She said: “I always thought drinking a few times a week was fine. I never knew it could raise my cancer risk. If I’d known earlier, I might have made different choices. Though hindsight is easy, my perspective has changed with the knowledge that came after my diagnosis.”
Drinking habits in the UK paint a concerning picture in comparison with other nations. Organisation for Economic Cooperation and Development (OECD) 2021 data showed that alcohol consumption in the UK was 10 litres per capita – 16% more than the OECD average of 8.6 litres.
Covid led to an increase in the number of high-risk drinks, with the heaviest drinkers increasing their consumption the most. These changes have persisted beyond the national lockdowns of 2020 and 2021, and subsequently there has been a year-on-year rise in alcohol-specific deaths, which reached an all-time high of 10,473 in 2023.
The research was conducted by Opinion Matters, among a sample of 2,000 nationally representative UK adults. The data was collected between 21.03.2025–24.03.2025.
Cancer Prevention Action Week (CPAW)
This year we’re highlighting the links between alcohol and cancer.
Alcohol and cancer: let’s talk – that was the theme of this year’s Cancer Prevention Action Week. For 7 days on 23–29 June, we talked to politicians, gave radio interviews and spoke to experts about alcohol and cancer. Plus, we shared news and views across our socials:
Facebook | LinkedIn | Instagram | Bluesky
How Cancer Prevention Action Week unfolded
Monday’s highlights
> Brits find it harder to talk about alcohol than sex or money
Yorkshire GP speaks out in support of CPAW:
Dr Nigel Wells, Medical Director and Executive Director Clinical & Care Professional Humber and North Yorkshire ICB and practising GP:
As a GP, I know people can be reluctant to talk about alcohol or share concerns about their drinking – so it doesn’t surprise me that only 2 in 10 people across Yorkshire and the Humber feel comfortable doing so.
But alcohol isn’t harmless – it increases the risk of 7 types of cancer, and, too often, people simply aren’t aware. If this campaign helps someone pause and ask whether alcohol might be affecting their health, and encourages them to speak to a healthcare professional, it will have made a real difference. We need to make these conversations as routine as those about smoking or diet – and that starts with creating a safe, non-judgemental space in every consultation.
We tabled an Early Day Motion in support of Cancer Prevention Action Week. And Alcohol Focus Scotland, a key supporter of this year’s campaign, tabled a motion in the Scottish Parliament on alcohol and cancer.
Tuesday’s highlights

Alcohol Focus Scotland organised a photo call at Holyrood with Members of the Scottish Parliament (MSPs). Photographed are 11 MSPs, including the Cabinet Secretary for Health Neil Gray; Jackie Baillie, Labour’s deputy leader and health spokesperson, and Presiding officer Alison Johnstone. Read more on LinkedIn
Sheridan Dixon, of South Tyneside, was interviewed on ITV Tyne Tees about how she has reduced her drinking as part of efforts to stay cancer free. We’re grateful to our partner Balance North East for helping us share Sheridan’s story.
Wednesday’s highlights

We headed to No 10 Downing St to present our petition to UK Prime Minister Sir Keir Starmer.
Prof Lord John Krebs, Chair of our Global Cancer Update Programme, tabled questions in the Lords on the links between alcohol and cancer, keeping the issue high on the political agenda:
Lord Krebs’ questions to the Lords
-
1
Lord Krebs to ask His Majesty’s Government what steps they are taking to reduce alcohol consumption as a modifiable risk factor for cancer.
-
2
Lord Krebs to ask His Majesty’s Government whether the national cancer plan for England will address alcohol consumption as a modifiable risk factor for cancer.
-
3
Lord Krebs to ask His Majesty’s Government what assessment they have made of public awareness levels of the link between alcohol consumption and cancer risk.
-
4
Lord Krebs to ask His Majesty’s Government what consideration they have given to classifying alcohol as an unhealthy product under high fat, sugar and salt marketing restrictions to (1) strengthen limits on alcohol advertising, and (2) reduce alcohol exposure among vulnerable populations, including children and adolescents.
-
5
Lord Krebs to ask His Majesty’s Government what assessment they have made of the impact of minimum unit pricing on alcohol-related cancer incidence.
CPAW supporter Prof Richard Cooke published research showing that policymakers and drinkers are speaking different languages when it comes to alcohol consumption. He says: “Policymakers need to construct policies to reflect the importance of emotions in drinkers’ narratives. This fits in with psychological theories of drinking behaviour which propose that people drink for different reasons.”
> The language of alcohol: Similarities and differences in how drinkers and policymakers frame alcohol consumption, published in Drug and Alcohol Review
Thursday’s highlights
Health professionals can be instrumental in helping individuals reset their relationship with alcohol and we supported them with a free webinar on Alcohol and cancer risk: What every health professional needs to know.
In the This Is Powerful podcast, Paul Sculfor talked to nutrition expert Dr Federica Amati about alcohol and cancer.
Friday’s highlights
On the blog: It’s mocktail Friday! Start your weekend early with some fizzy fruity creations
Saturday and Sunday’s highlights
Time to take a breath … alcohol is a major part of how many of us socialise, relax and celebrate. But nearly 4% of cancer cases in the UK are down to alcohol – around 17,000 new cases every year.
We hope this Cancer Prevention Action Week has given you an insight into the risks we’re all taking when we drink.
Our research shows that most people don’t know that drinking any amount of alcohol increases the risk of 7 types of cancer.
What happens next?
Cancer Prevention Action Week is just the start. We want to spark an ongoing national debate: with friends, family – and within government – about alcohol and cancer so that everyone can make more informed choices about their health.
But the UK government has said it won’t include mandatory comprehensive restrictions on alcohol marketing in its 10-year Health Plan – despite these being a proven, cost-effective way to reduce alcohol harm.
This is hugely disappointing. Contact the Prime Minister to make it clear that public health must be protected – and that cancer prevention cannot be sidelined.
On the blog
Media coverage
Cancer Prevention Action Week is across the news this week!
-
BBC Radio
Our Senior Policy Advisor, Kendra Chow, was invited to talk about this year’s campaign on BBC 5 Live on Saturday night. The interview was repeated across 5 Live and 43 other BBC radio stations.
-
Channel 5
Vanessa Feltz’s lunchtime show covered alcohol health warnings in a lengthy discussion including an interview with our supporter Dr Philippa Kaye.
Also on Channel 5, Jeremy Vine’s show discussed Alcohol labels should warn of cancer risk, urge health groups (The Times) in a round-up of the morning papers.
-
The Guardian
-
The Independent
-
The Times
-
The Telegraph
-
Julia Bradbury on Instagram
-
Scotland
-
International
- Mirage News (Australia)
- The Times of India
- Yahoo New Zealand
-
Science press
-
Trade press
-
Local press
- Rayo (Coventry and Nuneaton)
- This Is Wiltshire
- The Gazette and Herald
- Swindon Advertiser
- The Birmingham Mail
Facts at your fingertips
Written by experts, based on the evidence: our health resources unmuddle the myths about alcohol and cancer.
The government of the Republic of Ireland must ensure that the planned introduction of alcohol health labels, in May 2026, which are mandated under the Public Health (Alcohol) Act 2018, come into force without delay.
Dr Giota Mitrou, our Executive Director of Research and Policy, has written to Taoiseach Micheál Martin TD and Health Minister Jennifer Carroll MacNeill TD, in support of Ireland’s forthcoming mandatory health warnings labels on alcohol.
We are calling on the Irish government to stand firm on alcohol labelling in the face of misleading representations from the alcohol industry, and resist outside influence. Doing so, Dr Mitrou writes, will solidify Ireland’s record as a world leader on public health and set a much-needed example for other governments across the globe.
Health labels on alcohol crucial to preventing cancer
From 2026, all alcohol products sold in the Republic of Ireland will be required to state: “There is a direct link between alcohol and fatal cancers”. This measure makes Ireland the first country in the world to mandate a warning linking any level of alcohol consumption to cancer.
Yet Ireland is facing resistance to these measures from the alcohol industry in Ireland and worldwide.
Drinking any type of alcohol increases your risk of 7 different types of cancer, and our evidence shows that there is no safe level of drinking.
For Cancer Prevention Action Week 2025, on 23–29 June, we’re highlighting the links between alcohol and cancer and encouraging an open conversation about alcohol’s many harms.
> On the blog: How Ireland beat the odds to introduce cancer warning labels on alcohol
Dr Giota Mitrou
We strongly support alcohol health warning labels. This is not only an evidenced-based policy but also has immense public backing in Ireland, with 70% of those polled supportive of the measure. Crucially, the provision marks a significant step towards the Irish Government fulfilling their duty to protect the public from alcohol harm and reduce preventable cancers.
More on alcohol risks
World Cancer Research Fund has responded to the UK government’s first multi-year spending review, where the Chancellor, Rachel Reeves, set out departmental budgets over the next 3 years.
Under their Health Mission, the government has committed to shifting from sickness to prevention, affirming that prevention is better than cure. This spending review marks a critical opportunity for the government to set out their investment to this commitment.
In this review, the Chancellor committed:
- £29bn for the day-to-day spending of the NHS to 2028–29.
- £80m per year for tobacco cessation programmes and to support the delivery of the Tobacco & Vapes Bill.
- £10bn in NHS technology and digital transformation by 2028–29.
- £22.6bn per year for research and development by 2029–30, including medical research.
Responding to the spending review, World Cancer Research Fund’s Executive Director of Research and Policy, Dr Giota Mitrou, said:
Today the Chancellor reaffirmed Labour’s Health Mission, including their commitment to shift from treatment to prevention. 40% of all cancer cases are preventable: as leading experts in cancer prevention, we know that primary prevention remains the most sustainable and cost-effective way to tackle cancer and other non-communicable diseases.
For example, while we are glad to see that the government will be investing £80m per year to tackle tobacco, we need to see similar efforts applied to obesity and alcohol. The expansion of free school meals is a step in the right direction and the type of action we hope to see in the upcoming 10-year Health Plan.”