As part of Cancer Prevention Action Week 2025, on Wednesday we handed in an open letter and petition, alongside breast cancer survivors Dr Liz O’Riordan and Nikki Bednall, and the Alcohol Health Alliance.
The letter (below) – signed by more than 25 organisations and health experts – and the petition called on Prime Minister Sir Keir Starmer and his government to introduce a National Alcohol Strategy to Prevent Cancer, as part of our Cancer Prevention Action Week (CPAW) activity.
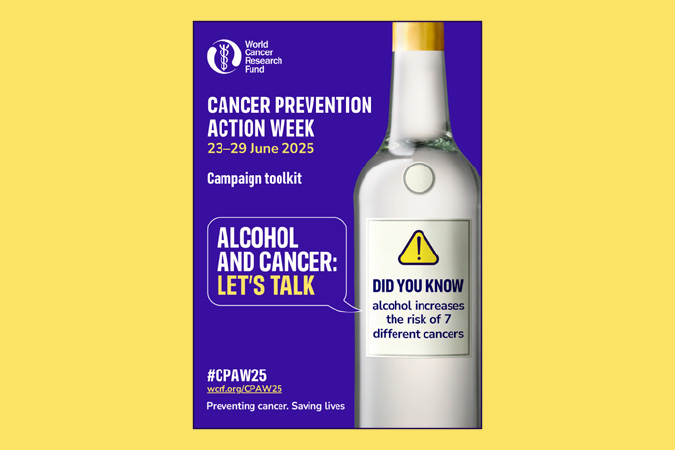
This year, CPAW is highlighting the links between alcohol and cancer – our research shows that most people don’t know that drinking any amount of alcohol increases the risk of 7 types of cancer.
What’s more, around 17,000 new cases every year are down to alcohol – so we’re urging the UK government to introduce a long-overdue National Alcohol Strategy for England – one that tackles alcohol harm head-on through:
- mandatory health warnings highlighting cancer risk
- minimum unit pricing
- marketing restrictions
to reduce consumption, lower cancer risk, and protect lives.





Read the full letter below
The Rt Hon Keir Starmer MP
Prime Minister
10 Downing Street
London SW1A 2AA
CC: The Rt Hon Wes Streeting MP, Secretary of State for Health and Social Care
Ashley Dalton MP, Parliamentary Under-Secretary of State for Public Health and Prevention
25 June 2025
The UK government must act on alcohol now to prevent cancer
Dear Prime Minister,
On behalf of more than 20 organisations and public health leaders, we are writing to share our deep concern about the continued lack of action to reduce alcohol consumption across the United Kingdom. In particular, the absence of a National Alcohol Strategy for England stands in stark contrast to the scale of harm caused by alcohol, with alcohol-specific deaths having increased by 42% in England between 2019 and 2023 alone.
This week marks Cancer Prevention Action Week (CPAW) – a national campaign led by World Cancer Research Fund (WCRF) – which seeks to empower the public and inspire change to prevent cancer. This year, CPAW is shining a spotlight on the link between alcohol and cancer, and the urgent need for government action.
In the UK, alcohol causes around 17,000 cases of cancer every year – equivalent to 46 people receiving a diagnosis every single day. And as our population ages and grows, these numbers are projected to rise. Worryingly, the pandemic has also driven an increase in high-risk drinking. Modelling by the Institute of Alcohol Studies and Health Lumen suggests that if this trend persists, we could see an additional 18,785 cancer cases by 2035.
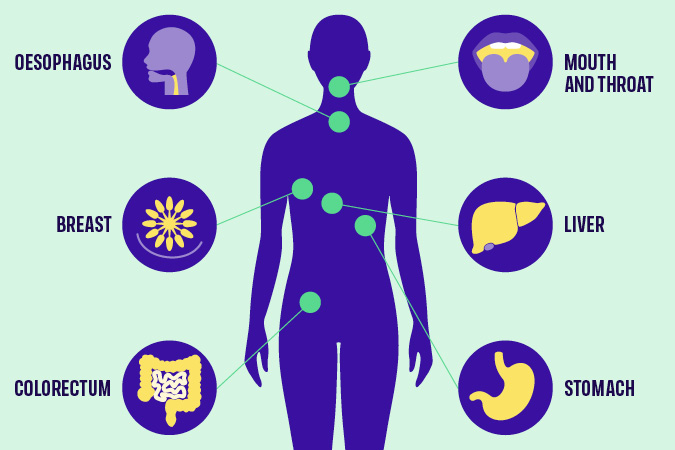
Public awareness remains alarmingly low that alcohol is a Group 1 carcinogen, the same category as tobacco and asbestos, and a cause of seven types of cancer, including two of the most common breast and bowel as well as mouth and throat, oesophageal, liver and stomach cancer. These risks are present even at low levels of consumption. New polling commissioned by WCRF reveals that when asked unprompted only 1 in 14 UK adults are aware that alcohol increases cancer risk and 25% believe there is no health risk attached to drinking alcohol.
We are not alone in our concern – thousands of members of the public including more than 20 organisations have signed our petition calling for greater government action. They agree that no one should have to suffer the devastating trauma of alcohol-related cancer.
The human toll is compounded by the economic burden. In 2016, Cancer Research UK estimated that alcohol-attributed cancers cost the NHS alone an estimated £100 million annually. With the health service under immense strain, it is imperative to act now and realise the government’s priority of prevention.
Despite alcohol being the sixth leading cause of preventable cancer in the UK, current policy does not reflect this reality. We urge the government to fulfil its responsibility to protect public health by introducing a National Alcohol Strategy for England without delay, which must include:
- Mandatory alcohol product labelling with health warnings, including information on cancer risks and calorie content.
- Marketing restrictions on alcohol by classifying it as an ‘unhealthy product’ under high fat, salt and sugar marketing restrictions.
- Implementing and evaluating minimum unit pricing at 65p in England with rates adjusted in line with inflation, to bring England into line with Scotland, Wales and Northern Ireland who all either have MUP already or have stated their intention to implement.
It is vital that this strategy aligns with the forthcoming National Cancer Plan for England, ensuring that alcohol is comprehensively addressed as a modifiable risk factor for cancer. We also urge the UK government to work in close collaboration with the devolved administrations, particularly to enable action to improve approaches to labelling and advertising. All policy development processes must be protected from industry influence and vested interests to ensure public health is placed above profit.
Such action would not only help to reduce cancer risks but reduce other alcohol-related harms. It would also support the government’s own ambitions to shift from sickness to prevention, as set out in the Health Mission, and contribute to economic growth by reducing illness-related inactivity.
We stand ready to support this effort and urge you to act now. Together we can tackle the devastating impact of both alcohol harm and cancer.
Yours sincerely,
Rachael Gormley, Chief Executive, World Cancer Research Fund
Dr Richard Piper, CEO, Alcohol Change UK
Alison Douglas, Chief Executive, Alcohol Focus Scotland
Professor Sir Ian Gilmore, Chair, Alcohol Health Alliance
Greg Fell, President, Association of Directors of Public Health
Dr Heather Grimbaldeston, Chair, BMA Public Health Medicine Committee, British Medical Association
Professor David Strain, Chair, BMA Board of Science, British Medical Association
Thalie Martini, Chief Executive Officer, Breast Cancer UK
Eddie Crouch, Chair, British Dental Association
Pamela Healy OBE, Chief Executive, British Liver Trust
Jill Clark, Chair, CancerWatch
Alison Wise, Communications Manager, on behalf of Fight Bladder Cancer
Ailsa Rutter OBE, Director, Fresh and Balance
Kostas Tsilidis, Associate Professor of Cancer Epidemiology and Prevention, Imperial College London
Dr Katherine Severi, Chief Executive, Institute of Alcohol Studies
Dr Dominique Florin, Medical Director, Medical Council on Alcohol
Daniela Binnington Nessman, Founder, Menopause and Cancer
Gopika Chandratheva, Nutritionist, NHS
Tamara Khan, CEO, Oracle Head & Neck Cancer UK
Jon Coleman-Reed, Head of Operations, Prevent Breast Cancer
Dr Claire Shannon, President, Royal College of Anaesthetists
Robert Steele, Chair, Board Directors, Scottish Cancer Foundation
Dr Alastair MacGilchrist, Chair, Scottish Health Action on Alcohol Problems
Chris Curtis, Chief Executive Officer, Swallows Head & Neck Cancer Support Charity
Amandine Garde, Professor of Law & Non-Communicable Diseases Research Unit, University of Liverpool
Richard Cooke, Professor of Health Psychology, University of Staffordshire
Dr Kathryn Scott, Chief Executive, Yorkshire Cancer Research
Only 16% of us in the UK feel at ease discussing our relationship with alcohol, ranking it among the least talked about topics – less so than sex (17%) and money (29%), according to our poll.
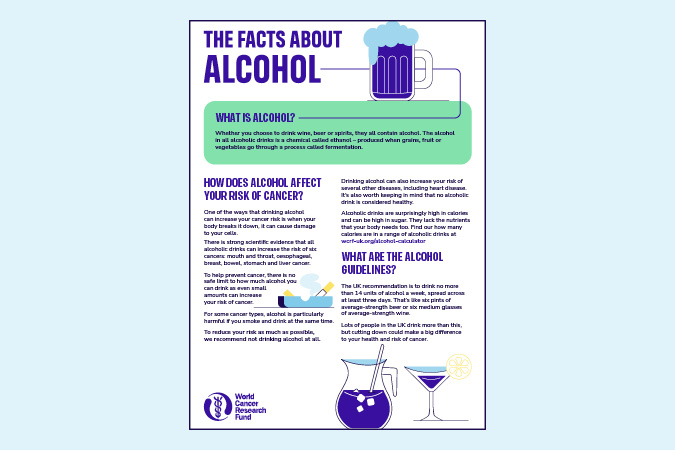
We’re emphasising the connection between alcohol and cancer as part of Cancer Prevention Action Week, which starts today. We have strong evidence that alcohol increases the risk of 7 cancers:
- Breast
- Bowel
- Head and neck
- Oesophageal
- Liver
- Stomach
Alcoholic drinks are also high in calories and often high in sugar, increasing the risk of gaining weight. Living with overweight or obesity increases the risk of at least 13 types of cancer.
We surveyed 2,000 people to gain insights into Britain’s understanding of alcohol and cancer risks. The findings reveal consistent misconceptions regarding alcohol’s dangers. Alarmingly, 25% of respondents did not associate any health risks with alcohol, and only 1 in 14 mentioned cancers as a risk when asked unprompted.
These misconceptions may hinder our ability to have informed conversations about alcohol. About 4% of cancer cases in the UK are attributed to alcohol, meaning that, each year, around 17,000 people are diagnosed with cancer caused by alcohol. Adding to this immeasurable human cost is the economic burden. Alcohol-related cancers cost the NHS around £100m every year.
We need a National Alcohol Strategy
We support clearer public health messaging to raise awareness of the real dangers of alcohol consumption, as well as other measures such as health warning labels. Alongside many other health organisations in the UK, we’re urging the Prime Minister, Sir Keir Starmer, to implement a National Alcohol Strategy for England.
World Cancer Research Fund CEO Rachael Gormley
Alcohol is pervasive in our lives, from celebrations to after-work drinks. But do we truly understand the risks involved? It’s essential that we engage in more discussions about alcohol and cancer, empowering individuals to make informed health choices.
Alcohol Health Alliance Chair Sir Ian Gilmore
One of the reasons public awareness is so low is that we're being kept in the dark about the true cost of drinking. People have the right to know the full picture so that they can make informed choices about what they consume.
World Cancer Research Fund Executive Director of Research and Policy Dr Giota Mitrou
A long-overdue National Alcohol Strategy in England would help the government tackle alcohol harm head on – reducing consumption, lowering cancer risk, and protecting lives.
Nikki Bednall is a World Cancer Research Fund Supporter and breast cancer survivor. She said: “I always thought drinking a few times a week was fine. I never knew it could raise my cancer risk. If I’d known earlier, I might have made different choices. Though hindsight is easy, my perspective has changed with the knowledge that came after my diagnosis.”
Drinking habits in the UK paint a concerning picture in comparison with other nations. Organisation for Economic Cooperation and Development (OECD) 2021 data showed that alcohol consumption in the UK was 10 litres per capita – 16% more than the OECD average of 8.6 litres.
Covid led to an increase in the number of high-risk drinks, with the heaviest drinkers increasing their consumption the most. These changes have persisted beyond the national lockdowns of 2020 and 2021, and subsequently there has been a year-on-year rise in alcohol-specific deaths, which reached an all-time high of 10,473 in 2023.
The research was conducted by Opinion Matters, among a sample of 2,000 nationally representative UK adults. The data was collected between 21.03.2025–24.03.2025.
Cancer Prevention Action Week (CPAW)
This year we’re highlighting the links between alcohol and cancer.
Alcohol and cancer: let’s talk – that was the theme of this year’s Cancer Prevention Action Week. For 7 days on 23–29 June, we talked to politicians, gave radio interviews and spoke to experts about alcohol and cancer. Plus, we shared news and views across our socials:
Facebook | LinkedIn | Instagram | Bluesky
How Cancer Prevention Action Week unfolded
Monday’s highlights
> Brits find it harder to talk about alcohol than sex or money
Yorkshire GP speaks out in support of CPAW:
Dr Nigel Wells, Medical Director and Executive Director Clinical & Care Professional Humber and North Yorkshire ICB and practising GP:
As a GP, I know people can be reluctant to talk about alcohol or share concerns about their drinking – so it doesn’t surprise me that only 2 in 10 people across Yorkshire and the Humber feel comfortable doing so.
But alcohol isn’t harmless – it increases the risk of 7 types of cancer, and, too often, people simply aren’t aware. If this campaign helps someone pause and ask whether alcohol might be affecting their health, and encourages them to speak to a healthcare professional, it will have made a real difference. We need to make these conversations as routine as those about smoking or diet – and that starts with creating a safe, non-judgemental space in every consultation.
We tabled an Early Day Motion in support of Cancer Prevention Action Week. And Alcohol Focus Scotland, a key supporter of this year’s campaign, tabled a motion in the Scottish Parliament on alcohol and cancer.
Tuesday’s highlights

Alcohol Focus Scotland organised a photo call at Holyrood with Members of the Scottish Parliament (MSPs). Photographed are 11 MSPs, including the Cabinet Secretary for Health Neil Gray; Jackie Baillie, Labour’s deputy leader and health spokesperson, and Presiding officer Alison Johnstone. Read more on LinkedIn
Sheridan Dixon, of South Tyneside, was interviewed on ITV Tyne Tees about how she has reduced her drinking as part of efforts to stay cancer free. We’re grateful to our partner Balance North East for helping us share Sheridan’s story.
Wednesday’s highlights

We headed to No 10 Downing St to present our petition to UK Prime Minister Sir Keir Starmer.
Prof Lord John Krebs, Chair of our Global Cancer Update Programme, tabled questions in the Lords on the links between alcohol and cancer, keeping the issue high on the political agenda:
Lord Krebs’ questions to the Lords
-
1
Lord Krebs to ask His Majesty’s Government what steps they are taking to reduce alcohol consumption as a modifiable risk factor for cancer.
-
2
Lord Krebs to ask His Majesty’s Government whether the national cancer plan for England will address alcohol consumption as a modifiable risk factor for cancer.
-
3
Lord Krebs to ask His Majesty’s Government what assessment they have made of public awareness levels of the link between alcohol consumption and cancer risk.
-
4
Lord Krebs to ask His Majesty’s Government what consideration they have given to classifying alcohol as an unhealthy product under high fat, sugar and salt marketing restrictions to (1) strengthen limits on alcohol advertising, and (2) reduce alcohol exposure among vulnerable populations, including children and adolescents.
-
5
Lord Krebs to ask His Majesty’s Government what assessment they have made of the impact of minimum unit pricing on alcohol-related cancer incidence.
CPAW supporter Prof Richard Cooke published research showing that policymakers and drinkers are speaking different languages when it comes to alcohol consumption. He says: “Policymakers need to construct policies to reflect the importance of emotions in drinkers’ narratives. This fits in with psychological theories of drinking behaviour which propose that people drink for different reasons.”
> The language of alcohol: Similarities and differences in how drinkers and policymakers frame alcohol consumption, published in Drug and Alcohol Review
Thursday’s highlights
Health professionals can be instrumental in helping individuals reset their relationship with alcohol and we supported them with a free webinar on Alcohol and cancer risk: What every health professional needs to know.
In the This Is Powerful podcast, Paul Sculfor talked to nutrition expert Dr Federica Amati about alcohol and cancer.
Friday’s highlights
On the blog: It’s mocktail Friday! Start your weekend early with some fizzy fruity creations
Saturday and Sunday’s highlights
Time to take a breath … alcohol is a major part of how many of us socialise, relax and celebrate. But nearly 4% of cancer cases in the UK are down to alcohol – around 17,000 new cases every year.
We hope this Cancer Prevention Action Week has given you an insight into the risks we’re all taking when we drink.
Our research shows that most people don’t know that drinking any amount of alcohol increases the risk of 7 types of cancer.
What happens next?
Cancer Prevention Action Week is just the start. We want to spark an ongoing national debate: with friends, family – and within government – about alcohol and cancer so that everyone can make more informed choices about their health.
But the UK government has said it won’t include mandatory comprehensive restrictions on alcohol marketing in its 10-year Health Plan – despite these being a proven, cost-effective way to reduce alcohol harm.
This is hugely disappointing. Contact the Prime Minister to make it clear that public health must be protected – and that cancer prevention cannot be sidelined.
On the blog
Media coverage
Cancer Prevention Action Week is across the news this week!
-
BBC Radio
Our Senior Policy Advisor, Kendra Chow, was invited to talk about this year’s campaign on BBC 5 Live on Saturday night. The interview was repeated across 5 Live and 43 other BBC radio stations.
-
Channel 5
Vanessa Feltz’s lunchtime show covered alcohol health warnings in a lengthy discussion including an interview with our supporter Dr Philippa Kaye.
Also on Channel 5, Jeremy Vine’s show discussed Alcohol labels should warn of cancer risk, urge health groups (The Times) in a round-up of the morning papers.
-
The Guardian
-
The Independent
-
The Times
-
The Telegraph
-
Julia Bradbury on Instagram
-
Scotland
-
International
- Mirage News (Australia)
- The Times of India
- Yahoo New Zealand
-
Science press
-
Trade press
-
Local press
- Rayo (Coventry and Nuneaton)
- This Is Wiltshire
- The Gazette and Herald
- Swindon Advertiser
- The Birmingham Mail
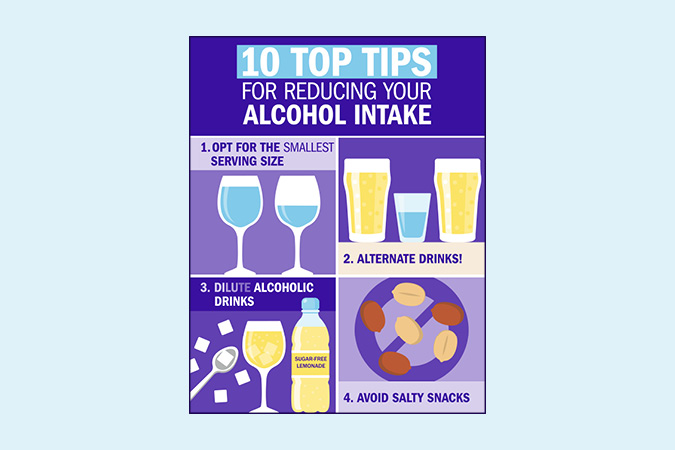
Facts at your fingertips
Written by experts, based on the evidence: our health resources unmuddle the myths about alcohol and cancer.
The government of the Republic of Ireland must ensure that the planned introduction of alcohol health labels, in May 2026, which are mandated under the Public Health (Alcohol) Act 2018, come into force without delay.
Dr Giota Mitrou, our Executive Director of Research and Policy, has written to Taoiseach Micheál Martin TD and Health Minister Jennifer Carroll MacNeill TD, in support of Ireland’s forthcoming mandatory health warnings labels on alcohol.
We are calling on the Irish government to stand firm on alcohol labelling in the face of misleading representations from the alcohol industry, and resist outside influence. Doing so, Dr Mitrou writes, will solidify Ireland’s record as a world leader on public health and set a much-needed example for other governments across the globe.
Health labels on alcohol crucial to preventing cancer
From 2026, all alcohol products sold in the Republic of Ireland will be required to state: “There is a direct link between alcohol and fatal cancers”. This measure makes Ireland the first country in the world to mandate a warning linking any level of alcohol consumption to cancer.
Yet Ireland is facing resistance to these measures from the alcohol industry in Ireland and worldwide.
Drinking any type of alcohol increases your risk of 7 different types of cancer, and our evidence shows that there is no safe level of drinking.
For Cancer Prevention Action Week 2025, on 23–29 June, we’re highlighting the links between alcohol and cancer and encouraging an open conversation about alcohol’s many harms.
> On the blog: How Ireland beat the odds to introduce cancer warning labels on alcohol
Dr Giota Mitrou
We strongly support alcohol health warning labels. This is not only an evidenced-based policy but also has immense public backing in Ireland, with 70% of those polled supportive of the measure. Crucially, the provision marks a significant step towards the Irish Government fulfilling their duty to protect the public from alcohol harm and reduce preventable cancers.
More on alcohol risks
Alcohol is a proven risk factor for 7 cancer types, and our evidence clearly shows there is no safe level of consumption when it comes to preventing cancer. Each year 17,000 people – 46 people every day – are diagnosed with a cancer caused by alcohol.
Alcohol deaths in England reached nearly 10,500 in 2023, a massive 42% increase since 2019. Despite these tragic statistics, alcohol policy across the UK remains woefully inadequate, doing very little to mitigate its significant harms, including cancer, and the immense burden it places on the NHS.
Making the case for change
Which cancers are linked to alcohol?
That’s why this year, our flagship campaign – Cancer Prevention Action Week – focuses on the links between alcohol and cancer, aiming to ensure that everyone can make informed decisions about their alcohol consumption. While raising awareness is important, it must be combined with evidenced-based polices that enable and support people to make healthier choices.
As many aspects of alcohol policy are the responsibility of the devolved administrations, Northern Ireland, Scotland and Wales all have alcohol strategies in place. In contrast, England has not had a National Alcohol Strategy since 2012.
We’re calling on the UK government to introduce a long overdue National Alcohol Strategy for England without delay. The Strategy must introduce policies on labelling, pricing and marketing – 3 interventions that have strong evidence of positive impact. Crucially, it must also remain independent of industry influence.
1) Labelling
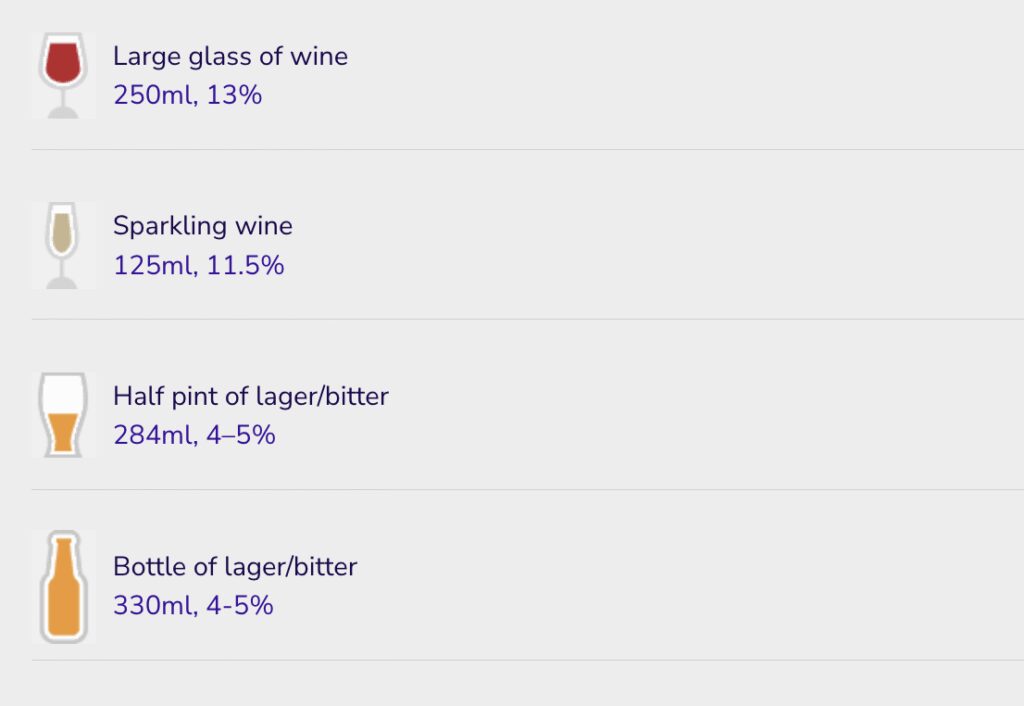
Despite being carcinogenic, alcohol is exempt from mandatory health warning labels. Unlike other food and drinks, alcohol labels are also not required to include information on nutritional content or calories. As the Alcohol Health Alliance puts it, there is more product information on a bottle of orange juice than on a bottle of beer. In fact, alcoholic drinks only have to display to display minimal information such as the name, strength as alcohol by volume (but only if over 1.2%), allergen information and the best before date (if the drink’s strength is under 10%). Even pregnancy and drink driving warnings are voluntary.
Consumers have a right to know about every product’s health risks and harms. Introducing health warning labels on alcohol that highlight cancer risk, alongside information on nutrition and calories, is an easy and effective way to ensure this. Evidence shows that effective labelling can prompt behaviour change and lead to reduced consumption.
For labelling to be effective, it must be clear, plain, distinct and mandatory. Additionally, labels should not include ambiguous language such as “drink responsibly”. Our policy position on alcohol explains that the use of QR codes to link to health information must be prohibited as, rather than informing people about risks, they provide marketing opportunities by redirecting consumers to producers’ websites.
2) Pricing
Minimum Unit Pricing (MUP) has been introduced in Scotland and Wales, but not in England or Northern Ireland. It sets a baseline price at which a unit of alcohol can be sold and targets cheap, strong alcohol that is often consumed by adolescents and other vulnerable groups.
Public Health Scotland’s review indicates that MUP has reduced alcohol-specific deaths by 13% and averted over 800 hospitals admissions every year since its introduction in 2012. MUP was found to have the most impact on those living in the 40% most deprived areas of Scotland, helping to reduce health inequalities. The Welsh government has also seen the benefits of MUP, which it introduced in 2020. Northern Ireland has consulted on proposals to introduce MUP.
England must follow suit, introducing MUP at 65p and adjusted for inflation thereafter. Without MUP in England, a 2.5 litre bottle of cider containing 19 units of alcohol can be bought for as little at £5.25. Under a 65p minimum unit price, this would rise to £12.19. Industry opposes MUP, arguing that it would damage sales in pubs and restaurants. However, most alcohol sold in these settings is already above minimum unit prices.
3) Marketing restrictions
Marketing restrictions on alcohol remain woefully inadequate. Advertising regulations prohibit linking alcohol with youth, irresponsible behaviour or social success, but enforcement is ineffective. The Advertising Standards Agency has no power to issue fines or sanctions, and often rules on complaints only after a campaign has ended. Like labelling, advertising is not a devolved issue, meaning the picture across the UK is largely the same.
Alcohol advertising is widespread, despite strong evidence linking exposure to alcohol marketing with young people drinking more and at an earlier age. The UK’s insufficient restrictions must be addressed by classifying alcohol as an “unhealthy product” under high fat, sugar or salt (HFSS) marketing restrictions. This would limit its promotion, particularly to vulnerable populations including children and adolescents.
The time to act is now
No family should have to endure the devastating trauma of alcohol-related cancer. Yet, as a result of the rise in high-risk drinking since the coronavirus pandemic, the UK could see more than 18,000 additional cancer cases by 2035.
Join us this Cancer Prevention Action Week to demand action. Sign and share our petition today, calling for a National Alcohol Strategy for England.
- The Alcohol Health Alliance, which we are a member of, has more information on MUP, labelling and marketing restrictions.
Get involved in Cancer Prevention Action Week
What is a UN High-Level Meeting?
A UN High-Level Meeting (HLM) is convened by the UN General Assembly. World leaders meet to agree actions to address a global issue. This year, the HLM will focus on the prevention and control of non-communicable diseases (NCDs) and mental health, and will be held on 25 September. It’s the 4th meeting to focus on NCDs, after meetings in 2011, 2014 and 2018. A Political Declaration, negotiated by Member States from May to September, will guide global commitments. This year’s HLM will need to address the insufficient progress made so far, and the urgent action needed to reduce the growing burden of NCDs, and improving mental health and wellbeing.
Addressing global burden of NCDs
NCDs cause 75% of global deaths, with 40% occurring before the age of 70. Low- and middle-income countries bear the greatest burden, with 82% of premature deaths. Cancer is the 2nd most common cause of NCD-related deaths, and cases are rising sharply. Only 19 countries are on track to meet SDG 3.4 by 2030 – risking over 6 million preventable deaths by then, and 40 million by 2060.
Unfortunately, previous HLMs on NCDs have failed to garner strong policy commitments from Member States, lacking specific targets, timelines, financial commitments, or accountability mechanisms – and each successive meeting has noted insufficient progress. This September’s HLM is crucial to reclaim these missed opportunities and achieve strong commitments on the prevention and control of NCDs now, and going forward. We will make the case to Member States on why prevention should be a key priority.
Approximately 40% of cancers are preventable, especially when modifiable risk factors are addressed. Incorporating prevention into the Political Declaration is vital to the success of the HLM as it offers the most effective and affordable long-term method of NCD and cancer control.
Prevention: high-impact and cost-effective
Countries must commit to bold, strategic and measurable targets in the Political Declaration to reduce rates of cancer. Activating prevention as a high-impact and cost-effective health intervention can support a future with fewer cases of cancer and NCDs, alongside fewer costs to human lives, health systems and economies. We have 5 key recommendations to be incorporated into the Political Declaration text:
- Speed up ‘Best Buy’ policy implementation Accelerating the implementation of evidence-backed policies like the WHO Best Buys – which focus on healthy diets, alcohol consumption, smoking and physical activity – would support a positive return on investment and improvements in population health.
- Implement National Cancer Control Plans, with prevention actions and indicators Only 30% of National Cancer Control Plans include prevention actions and indicators – a hugely missed opportunity. Integrating and financing national plans that prioritise prevention would be an effective, affordable and targeted strategy to reduce cancer incidence and improve outcomes.
- Invest in NCDs and prevention measures Financial and technical contributions need to be scaled up to match the global disease burden: NCDs cause 75% of global deaths, yet receive only 2% of development assistance. Every $1 invested in cost-effective interventions like the WHO Best Buys yields at least $7 in returns through better health, employment, productivity and economic stability.
- Address health inequities Cancer disproportionately affects marginalised and lower income populations, not only from higher mortality, but also through increased exposure to risk factors like health-harming products, such as unhealthy food and alcohol.
- Protect policymaking from health-harming industry interference Member States should commit to protecting policymaking processes from the influence of health-harming industries, and not allow lobbying activities to water down commitments that prioritise and protect health over corporate profits.
Action needed on NCDs – now
Much work needs to happen between now and the HLM in September. We’re attending the Multi-stakeholder Hearing in New York this week to engage Member States and share our priorities. Our advocacy will continue through our annual participation at the 78th WHO World Health Assembly this month, as we promote the benefits of cancer prevention policy.
We’ll participate in advocacy activities and side-events, promoting our HLM policy brief, which outlines our key messages. Civil society must continue its vital role in pushing for change and shaping an impactful Political Declaration.
We’ll collaborate with our longstanding partners such as NCD Alliance, UICC, World Obesity Federation and Movendi International to support the cancer and NCD prevention policy agenda. In the lead-up to the HLM in September, we’ll continue this series doing a deeper dive into each of these policy asks, and share our reflections as progress develops.
If you would be interested in supporting these advocacy asks, please reach out to policy@wcrf.org.
 We’ve come across many examples of human rights being used to advance cancer prevention at the McCabe Centre – whether through public interest litigation by civil society in south Asia to introduce smoke-free public places, or through incorporating non-communicable disease (NCD) prevention and healthy diets into regional human rights strategies and reporting to UN human rights bodies in the Pacific.
We’ve come across many examples of human rights being used to advance cancer prevention at the McCabe Centre – whether through public interest litigation by civil society in south Asia to introduce smoke-free public places, or through incorporating non-communicable disease (NCD) prevention and healthy diets into regional human rights strategies and reporting to UN human rights bodies in the Pacific.
We were therefore pleased to see World Cancer Research Fund International’s recently launched Policy Blueprint recognise the co-benefits of cancer prevention and the fulfilment of human rights.
This blog aims to explain what these co-benefits are, and how those working in cancer prevention can make the most of them.
Cancer prevention is part of our human rights
The International Covenant on Economic, Social and Cultural Rights establishes that people have a right, and countries have a duty, to prevention, treatment and control of disease as part of the right to health. The Committee on Economic, Social and Cultural Rights, which is established under the Covenant to assist in its interpretation, outlines that in order to protect, promote and fulfil the right to health, countries need to regulate health-harming products and make preventive health services and health information available, accessible, acceptable and good quality. The UN Special Rapporteur on the Right to Health, an independent expert on human rights whose mandate is established under the UN Human Rights Council, has endorsed a number of cancer prevention measures as a means of fulfilling this right, most specifically in relation to front-of-pack food labelling and promoting and supporting breastfeeding.
Likewise, the Committee on the Rights of the Child states that children’s right to health in the Convention on the Rights of the Child includes government obligations to address childhood obesity. This includes limiting children’s exposure to fast foods that are high in fat, sugar and salt or energy dense and nutrient poor, and regulating their marketing and availability in schools and other public places.
Grounding prevention policies in human rights
In many countries, human rights law can provide a valuable framing for engagement with ministries outside of health. In Argentina, civil society organisations successfully advocated for front-of-pack food labelling in parliament using a campaign strongly grounded in human rights. This included emphasising consumers’ right to information on whether foods had levels of sugar, fat and sodium that would harm health, and the right to healthier food environments as a component of the rights to food and health.
In Norway, the WHO’s guideline on policies to protect children from the harmful impact of food marketing, which is aligned with obligations under the Convention on the Rights of the Child, has been important to the Ministry of Health’s recent announcement of its plans to ban the marketing of junk foods to children.
The Committee on the Rights of the Child has raised concerns about commercial marketing in digital environments, including the profiling of children’s personal data for targeted marketing and the use of manipulative advertising techniques. The Committee has made recommendations that have been incorporated into UNICEF/WHO tools to support Member States to address the marketing of unhealthy foods to children. These connections between the marketing of unhealthy foods to children and a broader range of problematic digital commercial practices provide an opportunity to connect cancer prevention challenges to broader issues of online privacy, digital surveillance, and the rights of children in online spaces, and build alliances on these issues.
Cancer places an unequal burden on already marginalised or under-served communities, who are also more exposed to many cancer risk factors. A human rights approach, with its emphasis on ensuring that no one is left behind, and community participation and accountability, is a way of making sure that we have an equitable response that respects, protects and fulfils the rights of each individual to health. In her report on food, nutrition, and the right to health, the UN Special Rapporteur, Tlaleng Mofokeng, describes how disadvantaged groups are targeted in food marketing, and calls for more attention to be given to the relationship between NCDs, racial discrimination and gender.
Challenging the co-option of human rights by unhealthy industries
Despite human rights bodies’ recommendations to prevent cancer and regulate third parties’ impact on health, commercial interests such as the tobacco, alcohol or food industries are often more adept and better resourced at using this body of law than cancer prevention advocates. Unhealthy industries often invoke rights in litigation against public health laws, as part of a trend to launch legal challenges under trade, investment and constitutional law as a means of blocking public health policy. In Mexico, food companies launched a constitutional challenge to front-of-pack food labelling, arguing that it discriminated against food companies and restricted their right to trade.
Courts consistently reject these arguments, recognising that the rights of commercial actors must be balanced against other societal interests, including the rights of people to health, and that it does not enhance rights if we leave the marketing of harmful products by powerful commercial entities unchecked. The Supreme Court of Mexico upheld the front-of-pack labelling law, finding that the labels furthered the right to health and did not present a barrier to commerce. These challenges demonstrate the importance of proactively engaging with human rights and the law as part of a broader strategy on cancer prevention, so that lawyers representing commercial entities are less able to co-opt human rights to block public health policy.
A need for strategic alliances
Human rights are ultimately allies in implementing evidence-based laws to fulfil people’s right to health, with legal principles that emphasise equity, the right of consumers to be informed, and government obligations to regulate commercial actors that may harm human rights all fitting in well with public health objectives. Recalling these principles and building strategic alliances with human rights groups means we can better realise the potential of cancer prevention policies to promote and fulfil human rights for all.
The author would like to acknowledge Hayley Jones and Clare Slattery for comments on an earlier draft of this article.

Get the latest policy news first
Sign up to receive our monthly digest of nutrition and physical activity-related policy developments
In almost every region of the world, overweight and obesity among children and adolescents is a public health problem. There has been no progress in stemming the rate of overweight and obesity in children under 5 years in nearly 20 years, according to the World Health Organization (WHO).
This is a problem, because we know that when people live with overweight or obesity near the start of their lives, it often becomes a challenge throughout their adult lives.
What’s the problem with being inactive?
Young people may not be thinking very much about their risk of developing cancer. But the habits laid down in youth can last a lifetime. Our evidence shows that being active reduces the risk of colon (part of the bowel), post-menopausal breast and womb cancers.
Perhaps more importantly, being physically active also helps reduce our risk of living with overweight and obesity – a cause of at least 13 different types of cancer. Put simply, excess weight results from an imbalance between the energy we take in through our diet, and the energy we expend through being active (and other bodily functions). While we need to consider wider issues related to our ability to access a healthy diet, and managing stress and sleep levels, part of the solution involves being more active.
Are screens a particular problem?
Screens, and particularly mobile phones, have been blamed for a range of social and health problems among young people, including:
Evidence from our 2018 Diet and Cancer Report revealed convincing evidence that more screen time for children (from mobile phones but also using computers at school and watching devices during leisure time) makes weight gain more likely, as well as overweight and obesity.
The reasons for this are mixed. We tend to watch screens while sitting down, which uses less energy. Watching screens can also encourage us to eat more than is needed, not least because of exposure to adverts for unhealthy food and drinks, which young people may be particularly susceptible to.
The WHO lists limiting screen time as one of the ways to prevent and manage overweight and obesity in young people – but it’s only one.
What are the barriers to getting more active?

Young people’s experiences differ but, looking at the evidence and talking to parents and teenagers in the UK, a few common problems are highlighted:
- Underfunded / poor-quality equipment in public spaces (that may also feel unsafe to use).
- Cost – young people often don’t have a steady income, and gyms/clubs/sports can be expensive. Young people need access to parks and sports fields in their neighbourhoods.
- Travel – young people are often dependent on others for travel, which makes active travel – including safe routes to walk or cycle to school – and good public transport infrastructure so important (see below).
- Lack of options – children and young people in the UK are often offered activities such as football, netball and cross-country, but many want to try out less conventional sports such as yoga, dodgeball or trampolining.
- Gender – there is a significant decline in young girls taking part in sport, and parents of girls highlighted particular barriers to participation around body image, concerns about sweating and clothing, and lack of private changing spaces.
Elsewhere, a 2022 study looking at Botswana, Ethiopia, South Africa and Zimbabwe identified barriers around funding, but also highlighted community safety and a general lack of infrastructure as challenges.
What solutions are working around the world?
When developing ideas and designing policies to tackle overweight and obesity among children and young people, one voice is often unheard – that of young people themselves. From 2018–23, World Cancer Research Fund was involved in an innovative EU-funded project called CO-CREATE, which aimed to change that by putting young people at the forefront of tackling the obesity epidemic in Europe. The youth representatives on the project came up with 4 demands to policymakers, including “Offer all children and adolescents free, organized physical activities at least once every week.”
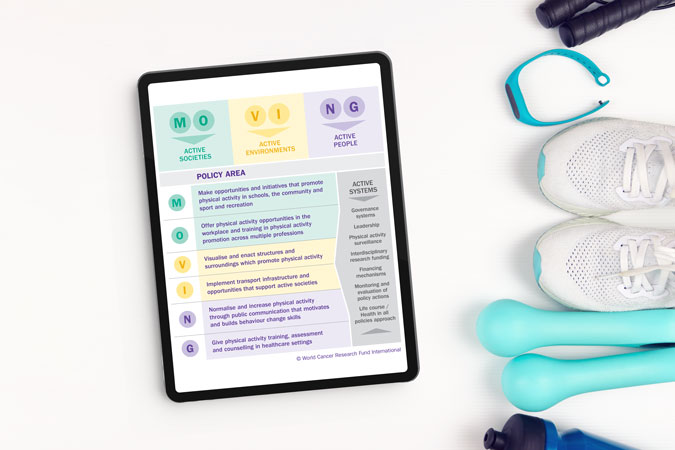
Using what they learned as part of the CO-CREATE project, our Policy team have devised a policy factsheet on physical activity, outlining the best ways to meet our Cancer Prevention Recommendation to be physically active.
Of all the information in the factsheet, some policy recommendations would specifically benefit children and young people, if acted on by governments around the world. These include:
- Initiatives that optimise opportunities for physical activity (including walking and cycling to and from school).
- Active play before and after school, as well as during recess and lunch breaks.
- Reduce sitting during classes.
- Policies to priorities active urban design, like ensuring access to open/green space or walking and cycling infrastructure where people live.
To keep people informed about both the need to be active, and the opportunities available to them, we also recommend:
- High quality physical education in school curricula.
- Enhanced physical activity training for all teachers.
And some of these innovative policies are already being undertaken in parts of the world. There are many policies recorded in our MOVING database mandating physical activity in schools, broadly ranging from 2–4 hours per week, depending on age and country.
And it’s not just dedicated PE sessions. Italy’s Scuola attiva kids aims to promote a culture of wellbeing and movement among not only students but teachers and families as well. In Finland, the Students on the Move programme encourages young people to sit less and move between breaks. Belgium’s Adventurous Activity initiative offers young people the chance to try out high and low ropes, tree climbing, rowing, BMX, skiing and orienteering.
Yet parents we spoke to suggested that there also needs to be a reframing of how PE is seen in school. One parent in Surrey, UK, said: “If you’re really good, you tend to do loads as part of a club, but there seems to be very little for those who aren’t any good.”
“There’s different aspects of sports. There’s one where you’re trying to create lifelong fitness for young people to engage in sport as part of a healthy lifestyle. And there’s another part where you need competitive sport to provide appropriate challenge” – Jennifer Cole, teacher and parent of 3, Brunei
“Emphasise fun so everyone can join in. Let people compete and win something but focus on beating personal bests rather than being top of the class so it’s not exclusive. Why not offer points or vouchers for those who increase their steps the most, not the ones with the overall highest numbers, so you’re encouraging people who don’t do anything?” – Mike, parent of 3 including 2 teenage girls, UK
Active travel was another key concern for parents – and is also one of our policy recommendations, including:
- Transport policies, systems and infrastructure that prioritise walking, cycling and use of public transport.
- Road safety actions for pedestrians and cyclists.
Active travel, which has the additional benefit of helping countries meet climate commitments, is already being promoted in many European countries. Austria’s Kindergarten Mobility Box aims to make walking and cycling the norm from a young age, and Belgium has similar scheme.
Perhaps, rather than just focusing on crisis-driven solutions to an increasingly inactive world, we need to listen more to young people about the changes they want to see in their world, alongside implementing policies that make it easier for everyone – especially young people – to move more and sit less as part of their everyday lives.
Want to get more active?
Check out our resources to help you get moving – written by experts
National Cancer Control Plans (NCCPs) are overarching strategic frameworks developed by governments to establish priorities for cancer, including:
- Prevention
- Diagnosis
- Treatment
- Survivorship
- Palliative care
Crucially, their potential to drive meaningful improvements in cancer outcomes has been proven.
Prevention is a glaring omission
The International Cancer Control Partnership’s most recent global review of NCCPs found that only 30% of all cancer plans address prevention. This is a glaring omission, especially given that the cancer burden is already unsustainable – placing increasing pressure on over-stretched health systems and economies. Nearly half (40%) of all cancer cases are preventable by addressing modifiable risk factors including diet, weight, activity, alcohol, smoking and sun exposures, underscoring the fact that prevention is the sustainable way forward.
World Cancer Research Fund are on a mission to wave the flag for primary prevention. First off, Rachael Gormley, acting president of World Cancer Research Fund International, took part in a roundtable event about NCCPs at the recent World Economic Forum in Davos, Switzerland. Rachael took full advantage of this important platform to emphasise why prevention must be central to all cancer strategies.
We also welcomed the UK government’s call for evidence on the National Cancer Plan for England. Our primary goal is to ensure that the new plan places prevention and survivorship at its heart. We’ll be sharing our written submission in due course and look forward to collaborating with organisations across sectors to amplify our calls.
Plans can be force for positive change

The International Cancer Benchmarking Partnership has examined the relationship between cancer policies and survival rates. It found significant potential for NCCPs to improve cancer diagnosis, treatment, and outcomes when applied strategically and successively.
Countries that adopt this approach have experienced the greatest improvements in cancer survival. For example, Denmark, which implemented 4 consecutive plans between 2000 and 2020, has significantly improved the survival rates for multiple cancers, including an 19% increase in the 1-year survival rate for lung cancer over 15 years.
Prevention is crucial to the success of NCCPs as it offers the most effective and affordable long-term method of cancer control. Prevention policies range from interventions aimed at reducing risk factors, such as helping smokers quit, and policies to reduce overweight and obesity, to actions that tackle cancer-causing infections, such as human papilloma virus vaccination programmes.
While NCCPs are not a silver bullet, they present a unique opportunity to implement targeted, context-specific actions on a national scale. This is particularly important for prevention, where wide-ranging strategies can benefit from the streamlined and coordinated structure of NCCPs, which can set out a roadmap of action across the entire prevention continuum.
Bottom line is rising cancer burden
The growing global cancer burden is why NCCPs focused on prevention are needed.
The WHO estimates that nearly 1 in 6 deaths globally are caused by cancer each year, meaning that annually around 10 million people lose their lives to cancer. The latest statistics on global cancer rates also show that in 2022, there were 20 million new cancer diagnoses, and 53.5 million people living with or beyond cancer.
The enormity of these figures can make it difficult to remember that they represent real people who have had their lives turned upside down by cancer.
It isn’t only the human cost of cancer that is immense. The social and economic costs are also undeniable, making it particularly concerning that globally new cases are expected to skyrocket to 35 million annually by 2050. This increase will be felt most acutely in low- and middle-income countries, which are expected to experience a more rapid rise in cancer rates in the coming decades.
Fortunately, this worrying trajectory is not inevitable. A focus on cancer prevention in NCCPs would allow millions more people to live cancer free. It is also the most cost-effective way to tackle cancer and, crucially, reduces the need for expensive later stage treatments that are often inaccessible to many. In addition, it could lead to an array of co-benefits such as the prevention of other non-communicable diseases and a reduction in health inequalities.
While this shift to prevention requires systemic change coupled with sustained investment, the challenge is not insurmountable. Ultimately investment in prevention will have the highest pay off for governments and the good news is that we already know the integrated policy approach needed to make this a reality.
NCCPs are a meaningful tool to prevent cancer and improve survivorship, support health systems, and promote economic growth. We will continue making the case for prevention to ensure that NCCPs fulfil their potential to reduce the cancer burden. Alongside working to ensure the National Cancer Plan for England prioritises prevention, we will be calling for all countries to develop NCCPs that include meaningful prevention measures at the UN High-Level Meeting on non-communicable diseases in September.
 Obesity is a public health emergency with England having one the highest rates among high-income nations.
Obesity is a public health emergency with England having one the highest rates among high-income nations.
There are stark inequalities in this country across the ages, geographic areas, genders, ethnic groups and for those with both mental and physical disabilities.
And these inequalities are growing, as rates of children with obesity are increasing significantly faster in communities with high deprivation levels compared to those with low deprivation levels.
And yet when the UK government has the chance to make a difference it is missing the mark.
They recently responded to the House of Lords Committee report entitled Recipe for Health, which set out realistic and transformative recommendations to improve the nation’s diet.
But we were disappointed to see their tepid response with the UK government listing their existing commitments rather than giving a clear signal that they would adopt any of the report’s recommendations.
This raises serious concerns about whether their upcoming National Food Strategy will turn out half-baked.
At World Cancer Research Fund, we want to see bold government policies in cancer prevention and nutrition.
This includes mandatory targets to improve nutritional quality of food, an expansion of the Soft Drinks Industry Levy to unhealthy foods as well as a strengthening of its sugar threshold, and the introduction of a mandatory front-of-pack labelling scheme.
The government must also ensure that the upcoming marketing restrictions on unhealthy foods are enforced without delay.
There is no doubt that the government wants to put prevention policies at the heart of what they do – they set it out clearly in their manifesto.
But with around 40% of cancer cases being preventable, they need to go further and faster on improving the nation’s diet – they need to take up the recommendations in the Recipe for Health report.

Our Cancer Prevention Recommendations
Experts now believe that up to 40% of cancer cases are preventable. These are a blueprint for how to reduce your risk of cancer
The International Agency for Research on Cancer estimates that, by 2050, the world will see 35 million new cancer cases each year, up by 15 million annual cases in 2022. Yet with the right policies to prevent cancer, 14 million of those people could avoid their diagnosis. These policies would need to address a variety of factors, including tobacco, alcohol, overweight and obesity, breastfeeding and unhealthy diet.
Cancer places increasing burden on society
As the cancer burden increases, the strain on our health systems, economies and families becomes harder to meet. Unhealthy weight – just one risk factor – is projected to cost the global economy more than $4 trillion a year by 2035. Our food systems make eating a healthier diet harder. High production and consumption of red and processed meat, and low consumption of wholegrains, vegetables, fruit and beans, plays a role in increased cancer risk and the risk of other diseases such as diabetes. This misalignment also contributes to unhealthy natural environments, as diet-related greenhouse gas emissions are significant contributors to global warming. Most of these are related to production of animal-based foods. This is why prevention is the only sustainable way forward – with resilient populations and food systems working together for public health.
Prevention the sustainable way forward
 We believe that prevention must be prioritised and is the only sustainable way forward. We also need to better explain:
We believe that prevention must be prioritised and is the only sustainable way forward. We also need to better explain:
- The science around cancer risk and diets, weight, breastfeeding, physical activity, and alcohol – as summarised in our Cancer Prevention Recommendations.
- Which policies should be prioritised to shape healthier environments that minimise these cancer risks for populations.
- How cancer prevention policy can have positive cascading effects for our health, but also for our health systems, our societies and our shared natural environment.
Cancer prevention policies can have ripple effect
We also know that cancer prevention policies can touch on and improve other areas beyond health. For example, diets high in red and processed meat increase people’s risk of colorectal cancer, and that healthier diets made up of more wholegrains, fruit and vegetables can protect people from the same type of cancer. This is why our Cancer Prevention Recommendations say people should limit red and processed meat, and eat a diet rich in wholegrains, vegetables, fruit and beansAt the same time, if our food systems produced less red and processed meat, and animal- food in general, and instead moved towards producing plant-based foods, this would have a significant impact in lowering diet-related CO2 emissions. Policymakers need to make sense of these connections, and our guidance shows what they need to do to promote such positive cycles – or co-benefits.
Why we created the Blueprint
Our well-established Cancer Prevention Recommendations cover 10 ways in which individuals can minimise their risk of preventable cancers. A growing body of evidence is showing that adherence to these Recommendations is associated with lower risk of developing cancer and other NCDs, but also lower risk of dying from cancer.
However, the Recommendations have not – until now – been presented alongside population-level policy advice. We need to promote an integrated approach to preventing cancer, otherwise policymakers may risk formulating repetitive but disconnected policy strategies across these areas that do not speak to or build on each other. For example, marketing restrictions can be a useful tool to encourage healthy diets but are also relevant for promoting breastfeeding and limiting alcohol consumption. Even though the targeted products are different, there are lessons to be learned from policy efforts across different cancer risk factors.
By joining the dots in these different areas, we can create greater awareness of how different policy approaches can contribute to cancer prevention. Our new blueprint makes a compelling case for action, especially for prevention to be included in national cancer plans. The blueprint also reinforces the need for a whole-of-government approach that puts public health goals before commercial interests.
What’s inside the Blueprint?
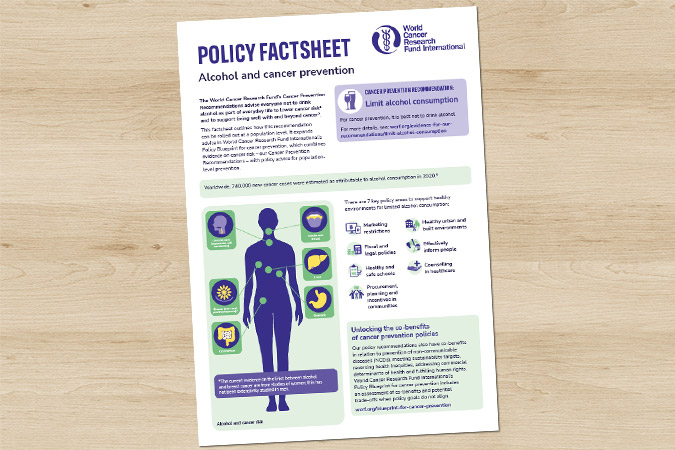
The Blueprint is accompanied by factsheets on specific cancer risk factors.
Our policy blueprint makes the case for population-level policy action and focuses on 5 factors: diet, weight, breastfeeding, physical activity and alcohol – in line with our Cancer Prevention Recommendations. We also look at how these factors can support people living with and beyond cancer
Our blueprint is an essential, evidence-based guide for policymakers and advocates, pulling together tools and resources to provide a comprehensive resource on cancer prevention. It pulls together existing tools and resources to support efforts on cancer prevention, including key guidance for World Health Organization, but also our existing NOURISHING nutrition and MOVING physical activity policy frameworks. All this information is distilled in a package of resources:
- An outline of 8 policy areas – including marketing restrictions, fiscal and legal, procurement, planning and incentives in communities– and how they apply to diet, weight, breastfeeding and physical activity.
- 10 factsheets with in-depth technical detail on how to roll out each Recommendation at population level.
- An exploration of the co-benefits of cancer prevention policy: addressing health inequities; meeting climate and sustainability targets; addressing commercial determinants of health; and fulfilling human rights.
- 7 strategies to help policymakers take action.
The goal of these resources is to strengthen understanding of how environment shapes cancer risk, and what policymakers can do about it.
How it was developed
To develop these resources, we built on our policy work, we reviewed existing key policy documents, and asked experts in the science and policy of cancer prevention, as well as lawyers, advocates for non-communicable disease prevention or breastfeeding what is most important in their respective areas. We then brought all the main elements together.
What’s next?
The Policy blueprint for cancer prevention will now be a centrepiece of our conversations with policymakers going forward – from Member States at the World Health Organization to the UN High-Level Meeting on Non-communicable diseases.
We invite you all to get involved: download the blueprint, share it, and use it in your work.
> Download our factsheets and other policy tools in our resource library
> To give us feedback and share how you want to use the blueprint, write to policy@wcrf.org
This year, we’ve been driving policy change to prevent cancer and improve public health globally and locally. Here are some of our highlights:
Global advocacy and engagement

Kendra Chow at WCC 2024
As part of our official relations status, we continue to work closely with the World Health Organization (WHO). This year was exceptionally busy as we expanded our engagement across 6 WHO teams and attended the Executive Board and World Health Assembly, where we made interventions (“statements”) across many agenda item areas.
- WHO Executive Board Statements: 7, including on wellbeing and health promotion, and social determinants of health.
- WHO World Health Assembly: delivered 6 impactful statements, 6 meetings with WHO officials and 5 meetings with civil society.
- WHO meetings: 5 meetings throughout the year with WHO staff to discuss collaboration.
- WHO consultations: contributed to 5 consultations including the WHO Director General report for the fourth UN High-Level Meeting (HLM) on non-communicable diseases (NCDs), and on Non-State Actors in official relations.
- Mission meetings and briefings: held meetings with 7 different country missions and developed 1 detailed mission briefing on our key priorities for the World Health Assembly.
Policy development and thought leadership
Our Alcohol and Cancer Risk brief
We advanced our policy work by publishing a major policy position, monitoring emerging issues, responding to consultations, contributing to a parliamentary inquiry, and launching new advocacy priorities in the UK. We’ve also continued to promote and advance our CO-CREATE project outputs.
- Published our comprehensive Alcohol and Cancer Risk policy position (which has been downloaded over 2,000 times!), along with a new dedicated section on our website.
- Monitored developments and engaged experts on the links between ultra-processed food and cancer.
- Responded to 1 international (on Norway’s forthcoming marketing restrictions) and 5 UK consultations (including the National Planning Policy Framework, which looks at how planning system can help our communities to be healthier).
- Provided evidence (PDF) to the House of Lord’s Select Committee on Food, Diet and Obesity.
- Introduced new policy priorities in the UK, strengthening our cancer prevention advocacy.
- 3 external partners utilised our NOURISHING and MOVING policy frameworks and tools, including the OECD, which used data from our NOURISHING and MOVING policy briefs for its 2024 report Beating Cancer Inequalities in the EU.
Communications and awareness
We enhanced our communications by redeveloping our website, producing podcasts and blogs, publishing newsletters, and co-signing advocacy letters to key policymakers.
- Redeveloped and revised all the Policy pages on our new website and developed a new resource library to house our statements, consultations, reports and policy tools.
- Featured in Movendi International’s podcast episode on How WCRFI Wants to Galvanize Governments to Address Alcohol’s Direct Link to Cancer.
- Published 10 blogs including a closer look at alcohol labelling, infant formula and baby foods, commercial determinants and this 2024 wrap-up.
- Published 13 monthly newsletters and newsflashes to over 1,100 subscribers.
- Endorsed 9 letters to the Prime Minister, Secretary of State for Health and Social Care, and Parliamentary Under-Secretary of State for Public Health and Prevention advocating policy change in the UK.
Collaboration and representation
We strengthened our advocacy by participating in major conferences, maintaining global research partnerships, hosting advisory meetings, and contributing to the development of key policy recommendations.
- Participated in 5 major conferences (European Congress on Obesity, World Cancer Congress, World Health Summit, International Society for Physical Activity and Health, European Public Health Conference). We also attended the Labour Party conference in the UK for the first time.
- Maintained valuable research partnerships with organisations around the world and hosted 2 Policy Advisory Group meetings.
- Continued contributing to the development of the policy recommendations that will accompany the forthcoming 5th European Code Against Cancer.
Team updates
We’ve had some changes in our team too.
Hellos and goodbyes: said farewell to Jennifer O’Mara, our Senior Policy and Public Affairs Officer, and Rebecca Taylor, our maternity cover Head of Policy and Public Affairs; and welcomed back our Head of Policy and Public Affairs Kate Oldridge-Turner. We look forward to our new Senior Policy and Public Affairs Officer, Melissa Dando, joining us in the new year.
Looking ahead to 2025
- We’re excited to launch our Policy Blueprint for Cancer Prevention in the new year – a new resource that draws together our Cancer Prevention Recommendations with our policy recommendations. Join us at the launch on 29 January 2025.
- Cancer Prevention Action Week: Join us for our week-long awareness raising campaign on alcohol and cancer risk in June 2025.
- We’ll be actively engaged in the 4th UN HLM on Non-Communicable Diseases, taking place in September 2025. Our focus will be for cancer prevention commitments to be included in the Political Declaration.
- 5th European Code Against Cancer: we’ll be supporting the launch of the new code in September 2025.
Thank you for your continued support – we are grateful for all the collaborations with our partners. Here’s to another year of impactful advocacy and policy work in 2025! Don’t forget you can sign up to our monthly newsletter straight into your inbox.