This year marks the 30th anniversary of the UK Women’s Cohort Study, the initial funding for which came from World Cancer Research Fund. Since its inception, this research – based at the University of Leeds – has grown into one of the largest and longest-running studies of diet and health in the UK. It continues to make a significant impact and serves as a foundation for ongoing research to this day.
The study was set up by Prof Janet Cade, who still works at University of Leeds. We’re looking forward to celebrating the study and its impact with her at a special event on Thursday 3 July 2025. We’d love to hear from any of the 35,000 women who were involved in this study, and would like to celebrate with us, Prof Cade and the team at Leeds.

Documents from the UK Women’s Cohort Study
Get involved
If you were part of the cohort, do contact Michael Clark on 020 7343 4205 or e-mail m.clark@wcrf.org to share your story or to be part of the celebrations.
Research funded by World Cancer Research Fund has shown that people living with cancer who closely follow a sustainable and nutritious diet – the EAT-Lancet reference diet – have a lower risk of dying from cancer and from all causes.
This is the first study to look at the impact of the EAT-Lancet diet on people living with or beyond cancer – as opposed to the general population. Prof Sabine Rohrmann and her team at the University of Zurich, in collaboration with colleagues from another Swiss university, the UK and Austria, used UK Biobank data to see if closely following this diet – with its emphasis on eating a rich variety of plant foods – affected the risk of death for people with a cancer diagnosis at the time they were recruited for the study.
Studying more than 25,000 people with an average age of 60 years at recruitment, the researchers used dietary information collected in the UK Biobank to develop a score that reflected how closely participants followed the EAT-Lancet diet.
More support needed for people facing cancer
Of the 25,348 cancer survivors in the group studied, 4,781 people died during the study follow-up. Prof Rohrmann’s results showed modest links between closely following the diet and a lower risk of dying from cancer, and of dying from all causes. The researchers didn’t observe a link between the diet and dying from heart disease.
Almost 64% of the participants were female, and participants who followed the EAT-Lancet diet more closely were more likely to be female. However, this study confirmed previous evidence showing that people living with and beyond cancer do not tend to follow healthy diets after their diagnosis. This emphasises the need to help people form healthier habits and overcome the barriers to eating well, such as treatment side-effects affecting appetite and taste.
These findings highlight the importance of greater nutrition support and guidance for people facing cancer. Guidelines aimed at the general population are unlikely to consider the needs of people living with and beyond cancer. With a lack of evidence-based recommendations for this population, the gap can sometimes be filled by practices not supported by the science – such as excessive use of dietary supplements.
This evidence showing the benefits of the EAT-Lancet diet follows recent research by our Global Cancer Update Programme, which provided guidance for people with a breast or a bowel cancer diagnosis.
Prof Sabine Rohrmann
We specifically put the focus of our study on cancer survivors because we believe that it is important to encourage them to follow a healthy lifestyle. For this, we need more evidence and so far, research on lifestyle changes in cancer survivors is still scarce.
Dr Julia Panina, Head of Research Funding
This study provides important new evidence that following the EAT-Lancet reference diet may reduce the risk of mortality in people living with and beyond cancer. The focus on the consumption of plant-based foods reflects our Cancer Prevention Recommendations to eat more wholegrains, vegetables, fruit and beans, and to limit red and processed meat. Importantly, these findings also show that diets supporting cancer survivorship can promote more sustainable eating and help protect the environment.
The EAT-Lancet reference diet was created by a team of scientists (The EAT-Lancet Commission on Food, Planet, Health) in 2019. It is a mainly plant-based diet that, according to the Commission, addresses the environmental impact of food production and consumption better than most national dietary guidelines.
> Read the paper: Higher adherence to the EAT-Lancet reference diet is inversely associated with mortality in a UK population of cancer survivors
> On the blog: Plant-based diets: eating for our health and the planet
Researchers funded by World Cancer Research Fund have discovered that brisk walking is linked to a lower risk of 5 cancers:
- anal
- liver (hepatocellular carcinoma)
- small intestine
- thyroid
- lung
Using information stored in the UK Biobank – a large database of many different aspects of health – scientists explored the link between walking pace – slow, steady or brisk – and the risk of developing 28 types of cancer.
They confirmed that the link between brisk walking and a reduced risk of developing the 5 cancers was true, even after accounting for overall physical activity and total walking time.
Speeding up your walk could represent an easy, low-cost public health intervention to decrease cancer risk.
The paper, published in BMC Cancer, says:
“Adopting a brisk walking pace may represent a pragmatic target for public health interventions to decrease cancer risk, particularly in circumstances where increases in walking volume or frequency prove impractical.”
PhD student Michael Stein’s research was supported by funding from Prof Michael Leitzmann’s grant. This research was funded by World Cancer Research Fund as part of the WCRF International Regular Grant Programme.
> Read the full paper: Usual walking Pace and risk of 28 cancers– results from the UK biobank
 John Steventon is our very own supporter superhero. He completed a HYROX in December dressed as comic book character Wolverine, alongside a friend who dressed as Deadpool – and he isn’t stopping there.
John Steventon is our very own supporter superhero. He completed a HYROX in December dressed as comic book character Wolverine, alongside a friend who dressed as Deadpool – and he isn’t stopping there.
HYROX is an indoor fitness race enhanced by workout stations along the route, so competitors run 1km, then do a workout – 8 times! The workouts include rowing, pulling and pushing a sled, and lunges while carrying a sandbag, making it an exhausting but fun challenge.
John said: “Everything I’ve done in life, I’ve wanted to share with others. As a DJ, I taught aspiring musicians and even wrote DJing for Dummies. In my TV career, I mentor new editors. When I was racing in indoor rowing, I launched the RowAlong YouTube channel to help home rowers stay motivated. So, when I started competing in HYROX, I wondered how I could use this platform to make a difference. “
“I knew I’d never be a podium finisher, but after my skin cancer diagnosis, I found a purpose: racing as Wolverine to raise money for World Cancer Research Fund. The response from the HYROX community has been incredible – not just in donations, but in the conversations I’ve had. Nearly everyone I meet has been touched by cancer in some way, whether personally or through friends and family.”
‘I thought I was invincible’
“Even though the doctor said, “Don’t worry”, when I heard the words “That’s skin cancer” the last hope that I was indestructible fizzled away. I’d always thought I was invincible – after all, I like to dress up as Wolverine – but skin cancer reminded me that none of us are.”
John’s diagnosis helped him become more aware of the importance of cancer prevention. “I remember being 7 years old, resisting my Mum’s attempts to put sun cream on me. I often opted for the lowest SPF possible, thinking sunburn was just a fast track to a tan. Coming from Scotland, where sunshine is a rarity, I’ve always craved the sun’s warmth. But now, I never go without factor 30 or 50. If only I had learned that lesson earlier.
“The guidance from the World Cancer Research Fund has been invaluable in helping me understand the importance of proper nutrition and lifestyle choices in cancer prevention and overall health. Exercise alone isn’t enough – we need to fuel ourselves properly and protect ourselves from preventable risks like excessive sun exposure.”
John continues to take on HYROX challenges to raise money for us. He’s completed 3, including one in Frankfurt, and is running The Grid competition again in September, as well as more HYROX events this year. So far, he’s raised nearly £2,000 towards cancer prevention – thank you, John!
Having a greater weight at birth, or a higher body size as a child, adolescent or young adult, is associated with an increased risk of bowel cancer (also known as colorectal cancer) in later life, according to new analysis by World Cancer Research Fund International.
In a major review, looking at 37 studies, our experts discovered that a higher body mass index (BMI) in childhood (2–9 years), adolescence (10–19 years), and young adulthood (18–25 years) increased bowel cancer risk during adulthood. A higher birthweight was also associated with a higher bowel cancer risk.
Innovative research
This work is part of our Global Cancer Update Programme (CUP Global). The paper is published today in the International Journal of Cancer.
The review was conducted by researchers at Wageningen University & Research (WUR) in the Netherlands. It is the first review to analyse and judge all the research examining how factors such as weight, height and body size in early life relate to our risk of bowel cancer as we get older. The results of the study were judged by our CUP Global Expert Panel.
> More information about how we judge the evidence and our evidence grading criteria.
Dr Helen Croker, Assistant Director of Research and Policy
Cancer is a complex disease which develops over several decades, so better understanding of its early origins is critical for more effective prevention and understanding the research gaps. This study shows that a higher body mass index across childhood through young adulthood is an important risk factor for colorectal cancer.
Dr Dieuwertje Kok, Associate Prof of Nutrition and Cancer at WUR
The team was excited to review results from 37 publications that explored birthweight, as well as body mass index across different early life stages. This study bridges the existing knowledge gap and enhances our understanding of how early life factors may affect colorectal cancer risk in adults.
CUP Global is the world’s largest and most authoritative source of research on cancer prevention and living with and beyond cancer. It’s a rigorous, systematic programme that gathers, analyses and assesses global research on how diet, nutrition, physical activity and body weight affect cancer risk and survival.
CUP Global is funded by the World Cancer Research Fund network of charities: American Institute for Cancer Research, World Cancer Research Fund and Wereld Kanker Onderzoek Fonds (WKOF). The review informing this work was funded by WKOF through a CUP Global collaboration with WUR.
Our research portfolio spans a wide range of areas within cancer prevention. Today we’re spotlighting a lab-based study taking place in Newcastle. Local MP Chi Onwurah met Assoc Professor Jill McKay, Prof Dianne Ford and Dr Jessica Saville from Northumbria University, to discuss their groundbreaking cancer prevention research.
Hosted at the university, Chi learned about cancer prevention at the molecular level through her engagement with Assoc Prof Jill McKay and her team. World Cancer Research Fund awarded the team a £347,000 grant to conduct a laboratory-based study investigating whether folate levels in expectant mothers are linked to the development of leukaemia in their children. Folate is a B-vitamin naturally found in green leafy vegetables and liver, while its synthetic form, folic acid, is commonly used in supplements and fortified foods. Some studies suggest folic acid supplementation during pregnancy may help prevent childhood leukaemia; however, findings are not yet clear.
Leukaemia, a cancer of the blood, is the most common childhood cancer worldwide, responsible for 1 in 3 childhood cancers, and rates are slowly increasing. This important research could identify biological markers to help screen or monitor children at increased risk. Ultimately this could lead to earlier diagnosis, which is closely tied to better outcomes for leukaemia patients. It could also result in improved nutritional guidelines for pregnancy.
Assoc Prof Jill McKay, Principal investigator, Northumbria University
Rates of childhood leukaemia are slowly rising, which suggests some things in our environment may be contributing to this disease developing. Learning more about what factors can affect leukaemia and how they influence underlying biology can help us know which lifestyle changes we can make to aim to prevent and predict childhood leukaemia. However, none of this will be possible unless we liaise with policy makers, so we are delighted to meet with Chi today to share our exciting research.
Importantly, the researchers and MP discussed the study’s potential to influence nutritional guidelines during pregnancy, reduce the risk of childhood leukaemia, and support earlier diagnosis. As Chair of the Science, Innovation and Technology Committee, Chi Onwurah MP was particularly interested in hearing about the study’s progress, upcoming publications, and future plans following its completion.
Dr Jana Sremanakova, Research Funding Manager, WCRF International
This is a particularly exciting and important moment for us at the World Cancer Research Fund, as it marks the first time we are connecting our grant holders directly with their MP. It’s a unique opportunity to highlight the impact of our work in cancer prevention research and our national cancer prevention efforts.
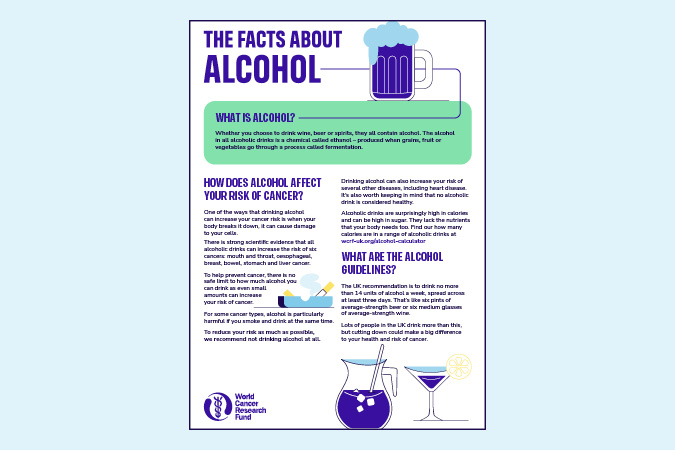
Alcohol is a proven risk factor for 7 cancer types, and our evidence clearly shows there is no safe level of consumption when it comes to preventing cancer. Each year 17,000 people – 46 people every day – are diagnosed with a cancer caused by alcohol.
Alcohol deaths in England reached nearly 10,500 in 2023, a massive 42% increase since 2019. Despite these tragic statistics, alcohol policy across the UK remains woefully inadequate, doing very little to mitigate its significant harms, including cancer, and the immense burden it places on the NHS.
Making the case for change
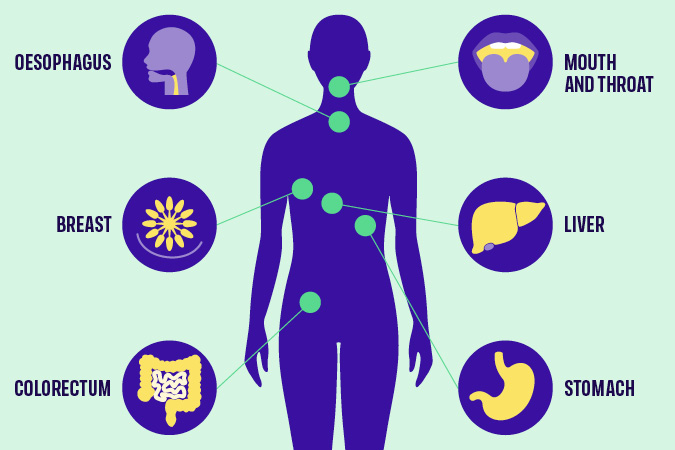
Which cancers are linked to alcohol?
That’s why this year, our flagship campaign – Cancer Prevention Action Week – focuses on the links between alcohol and cancer, aiming to ensure that everyone can make informed decisions about their alcohol consumption. While raising awareness is important, it must be combined with evidenced-based polices that enable and support people to make healthier choices.
As many aspects of alcohol policy are the responsibility of the devolved administrations, Northern Ireland, Scotland and Wales all have alcohol strategies in place. In contrast, England has not had a National Alcohol Strategy since 2012.
We’re calling on the UK government to introduce a long overdue National Alcohol Strategy for England without delay. The Strategy must introduce policies on labelling, pricing and marketing – 3 interventions that have strong evidence of positive impact. Crucially, it must also remain independent of industry influence.
1) Labelling
Despite being carcinogenic, alcohol is exempt from mandatory health warning labels. Unlike other food and drinks, alcohol labels are also not required to include information on nutritional content or calories. As the Alcohol Health Alliance puts it, there is more product information on a bottle of orange juice than on a bottle of beer. In fact, alcoholic drinks only have to display to display minimal information such as the name, strength as alcohol by volume (but only if over 1.2%), allergen information and the best before date (if the drink’s strength is under 10%). Even pregnancy and drink driving warnings are voluntary.
Consumers have a right to know about every product’s health risks and harms. Introducing health warning labels on alcohol that highlight cancer risk, alongside information on nutrition and calories, is an easy and effective way to ensure this. Evidence shows that effective labelling can prompt behaviour change and lead to reduced consumption.
For labelling to be effective, it must be clear, plain, distinct and mandatory. Additionally, labels should not include ambiguous language such as “drink responsibly”. Our policy position on alcohol explains that the use of QR codes to link to health information must be prohibited as, rather than informing people about risks, they provide marketing opportunities by redirecting consumers to producers’ websites.
2) Pricing
Minimum Unit Pricing (MUP) has been introduced in Scotland and Wales, but not in England or Northern Ireland. It sets a baseline price at which a unit of alcohol can be sold and targets cheap, strong alcohol that is often consumed by adolescents and other vulnerable groups.
Public Health Scotland’s review indicates that MUP has reduced alcohol-specific deaths by 13% and averted over 800 hospitals admissions every year since its introduction in 2012. MUP was found to have the most impact on those living in the 40% most deprived areas of Scotland, helping to reduce health inequalities. The Welsh government has also seen the benefits of MUP, which it introduced in 2020. Northern Ireland has consulted on proposals to introduce MUP.
England must follow suit, introducing MUP at 65p and adjusted for inflation thereafter. Without MUP in England, a 2.5 litre bottle of cider containing 19 units of alcohol can be bought for as little at £5.25. Under a 65p minimum unit price, this would rise to £12.19. Industry opposes MUP, arguing that it would damage sales in pubs and restaurants. However, most alcohol sold in these settings is already above minimum unit prices.
3) Marketing restrictions
Marketing restrictions on alcohol remain woefully inadequate. Advertising regulations prohibit linking alcohol with youth, irresponsible behaviour or social success, but enforcement is ineffective. The Advertising Standards Agency has no power to issue fines or sanctions, and often rules on complaints only after a campaign has ended. Like labelling, advertising is not a devolved issue, meaning the picture across the UK is largely the same.
Alcohol advertising is widespread, despite strong evidence linking exposure to alcohol marketing with young people drinking more and at an earlier age. The UK’s insufficient restrictions must be addressed by classifying alcohol as an “unhealthy product” under high fat, sugar or salt (HFSS) marketing restrictions. This would limit its promotion, particularly to vulnerable populations including children and adolescents.
The time to act is now
No family should have to endure the devastating trauma of alcohol-related cancer. Yet, as a result of the rise in high-risk drinking since the coronavirus pandemic, the UK could see more than 18,000 additional cancer cases by 2035.
Join us this Cancer Prevention Action Week to demand action. Sign and share our petition today, calling for a National Alcohol Strategy for England.
- The Alcohol Health Alliance, which we are a member of, has more information on MUP, labelling and marketing restrictions.
Get involved in Cancer Prevention Action Week
Seed oils are made by extracting oil from the seeds of various plants, such as:
- Sunflower
- Rapeseed (also known as canola oil)
- Sesame
- Grape
- Flax
- Soybean
- Safflower
These oils are versatile and many are budget-friendly choices in the kitchen. Most have a neutral flavour and a high smoke point, which means they can handle high cooking temperatures – like when you’re frying or roasting – without breaking down or producing unpleasant flavours or potentially harmful compounds. This makes them a safer and more reliable option for everyday cooking.
A particular benefit of seed oils is that they are high in unsaturated fat – the type we should eat more of – and low in saturated fat, which we should eat less of. This makes them a healthier alternative to animal fats like butter and ghee.
Importantly, seed oils provide essential omega-6 fats, which our bodies can’t make so we need them from our diet. These fats support healthy skin, and help build and maintain our cells.
Seed oils and inflammation

You may have seen claims that seed oils cause inflammation. This is mainly because they contain an omega-6 fat called linoleic acid, which can be converted in small amounts into another fat called arachidonic acid – a compound involved in the body’s inflammatory response.
Some people worry that eating too much omega-6 could compete with omega-3 fats, which support heart and brain health, and have anti-inflammatory properties. The concern is that both fats share some pathways in the body, so too much omega-6 may reduce the impact of omega-3s and promote inflammation.
But research doesn’t support this idea. In fact, studies show that people who eat more linoleic acid – the type found in seed oils – often have lower levels of inflammatory markers in the body. Instead of cutting back on omega-6, it’s more important to focus on getting enough omega-3s in your diet by eating oily fish (like salmon), green leafy vegetables (like brussels sprouts) and nuts (like walnuts).
What about cancer risk?
When it comes to cancer, there’s no strong evidence to show that seed oils increase risk. What matters most is your overall diet – we recommend you eat a diet rich in fruit, vegetables, wholegrains, pulses, nuts, seeds and lean proteins like fish and chicken to support your long-term health and reduce cancer risk.
Seed oils in processed foods
Seed oils can be found in ultra-processed products like:
- shop-bought salad dressings
- mayonnaise
- cakes
- biscuits
- crisps
- sweet and savoury pastries
These foods are typically high in salt and sugar, and low in fibre, vitamins and minerals – not ideal for our health.
In fast food restaurants, oils may be reheated multiple times at very high temperatures, which can produce potentially harmful compounds. Most of us don’t cook like that at home.
But it’s important to remember – seed oils themselves aren’t the problem. The real issue is the overall quality of the processed foods that contain them. It’s these foods that are linked to a higher risk of obesity, heart disease, type 2 diabetes and some cancers.
That’s why one of our Cancer Prevention Recommendations is to limit fast food and processed foods that are high in saturated fat, salt and sugar.
So, should I avoid seed oils?
Not at all – and there’s no need to fear them. Seed oils can be part of a healthy, balanced diet. They’re low in saturated fat, provide essential omega-6 fats and offer useful nutrients like vitamins E and K, which support immune health and normal blood clotting.
As with all fats, it’s about using them wisely. They’re high in calories, so stick to small amounts – a teaspoon or a light spray is often all you need. Seed oils are versatile in the kitchen, perfect for roasting, stir-fries, baking, homemade salad dressings or as a healthier alternative to butter or ghee.
References
-
List of journals consulted
Johnson GH, Fritsche K. Effect of dietary linoleic acid on markers of inflammation in healthy persons: a systematic review of randomized controlled trials. Journal of the Academy of Nutrition and Dietetics [Internet]. 2012 Jun 21;112(7):1029-1041.e15.
Laurindo LF, Laurindo LF, Rodrigues VD, Da Silva Camarinha Oliveira J, Boaro BL, Araújo AC, et al. Evaluating the effects of seed oils on lipid profile, inflammatory and oxidative markers, and glycemic control of diabetic and dyslipidemic patients: a systematic review of clinical studies. Frontiers in Nutrition [Internet]. 2025 Feb 7;12.
Petersen KS, Maki KC, Calder PC, Belury MA, Messina M, Kirkpatrick CF, et al. Perspective on the health effects of unsaturated fatty acids and commonly consumed plant oils high in unsaturated fat. British Journal of Nutrition [Internet]. 2024 Oct 28;132(8):1039–50.
Pischon T, Hankinson SE, Hotamisligil GS, Rifai N, Willett WC, Rimm EB. Habitual Dietary Intake of n-3 and n-6 Fatty Acids in Relation to Inflammatory Markers Among US Men and Women. Circulation [Internet]. 2003 Jun 24;108(2):155–60.
Rett BS, Whelan J. Increasing dietary linoleic acid does not increase tissue arachidonic acid content in adults consuming Western-type diets: a systematic review. Nutrition & Metabolism [Internet]. 2011 Jan 1;8(1):36.
Su H, Liu R, Chang M, Huang J, Wang X. Dietary linoleic acid intake and blood inflammatory markers: a systematic review and meta-analysis of randomized controlled trials. Food & Function [Internet]. 2017 Jan 1;8(9):3091–103.
What is a UN High-Level Meeting?
A UN High-Level Meeting (HLM) is convened by the UN General Assembly. World leaders meet to agree actions to address a global issue. This year, the HLM will focus on the prevention and control of non-communicable diseases (NCDs) and mental health, and will be held on 25 September. It’s the 4th meeting to focus on NCDs, after meetings in 2011, 2014 and 2018. A Political Declaration, negotiated by Member States from May to September, will guide global commitments. This year’s HLM will need to address the insufficient progress made so far, and the urgent action needed to reduce the growing burden of NCDs, and improving mental health and wellbeing.
Addressing global burden of NCDs
NCDs cause 75% of global deaths, with 40% occurring before the age of 70. Low- and middle-income countries bear the greatest burden, with 82% of premature deaths. Cancer is the 2nd most common cause of NCD-related deaths, and cases are rising sharply. Only 19 countries are on track to meet SDG 3.4 by 2030 – risking over 6 million preventable deaths by then, and 40 million by 2060.
Unfortunately, previous HLMs on NCDs have failed to garner strong policy commitments from Member States, lacking specific targets, timelines, financial commitments, or accountability mechanisms – and each successive meeting has noted insufficient progress. This September’s HLM is crucial to reclaim these missed opportunities and achieve strong commitments on the prevention and control of NCDs now, and going forward. We will make the case to Member States on why prevention should be a key priority.
Approximately 40% of cancers are preventable, especially when modifiable risk factors are addressed. Incorporating prevention into the Political Declaration is vital to the success of the HLM as it offers the most effective and affordable long-term method of NCD and cancer control.
Prevention: high-impact and cost-effective
Countries must commit to bold, strategic and measurable targets in the Political Declaration to reduce rates of cancer. Activating prevention as a high-impact and cost-effective health intervention can support a future with fewer cases of cancer and NCDs, alongside fewer costs to human lives, health systems and economies. We have 5 key recommendations to be incorporated into the Political Declaration text:
- Speed up ‘Best Buy’ policy implementation Accelerating the implementation of evidence-backed policies like the WHO Best Buys – which focus on healthy diets, alcohol consumption, smoking and physical activity – would support a positive return on investment and improvements in population health.
- Implement National Cancer Control Plans, with prevention actions and indicators Only 30% of National Cancer Control Plans include prevention actions and indicators – a hugely missed opportunity. Integrating and financing national plans that prioritise prevention would be an effective, affordable and targeted strategy to reduce cancer incidence and improve outcomes.
- Invest in NCDs and prevention measures Financial and technical contributions need to be scaled up to match the global disease burden: NCDs cause 75% of global deaths, yet receive only 2% of development assistance. Every $1 invested in cost-effective interventions like the WHO Best Buys yields at least $7 in returns through better health, employment, productivity and economic stability.
- Address health inequities Cancer disproportionately affects marginalised and lower income populations, not only from higher mortality, but also through increased exposure to risk factors like health-harming products, such as unhealthy food and alcohol.
- Protect policymaking from health-harming industry interference Member States should commit to protecting policymaking processes from the influence of health-harming industries, and not allow lobbying activities to water down commitments that prioritise and protect health over corporate profits.
Action needed on NCDs – now
Much work needs to happen between now and the HLM in September. We’re attending the Multi-stakeholder Hearing in New York this week to engage Member States and share our priorities. Our advocacy will continue through our annual participation at the 78th WHO World Health Assembly this month, as we promote the benefits of cancer prevention policy.
We’ll participate in advocacy activities and side-events, promoting our HLM policy brief, which outlines our key messages. Civil society must continue its vital role in pushing for change and shaping an impactful Political Declaration.
We’ll collaborate with our longstanding partners such as NCD Alliance, UICC, World Obesity Federation and Movendi International to support the cancer and NCD prevention policy agenda. In the lead-up to the HLM in September, we’ll continue this series doing a deeper dive into each of these policy asks, and share our reflections as progress develops.
If you would be interested in supporting these advocacy asks, please reach out to policy@wcrf.org.
- Report provides further clarity on dietary and lifestyle pattern (DLP) recommendations for breast and colorectal cancer prevention following a comprehensive review of 170 global studies
- Adopting a healthy DLP could also have important environmental and societal benefits, say report authors, and more can be done by policymakers to support adopting a healthy, cancer preventative DLP adoption globally
World Cancer Research Fund (WCRF) International has released a major new report on DLPs and their role in cancer prevention – out today (9 April 2025).
Today’s report emphasises that studying DLPs together, rather than looking at single foods or behaviours, can help researchers and the public to better understand how all these factors together play a role in reducing cancer risk.
An independent panel of experts reviewed the available global evidence on dietary and lifestyle patterns and breast and colorectal cancer. The evidence – which was judged to be strongly associated with cancer risk – was used to develop our new recommendation of a cancer preventative DLP.
What are dietary and lifestyle patterns?
Dietary patterns refer to quantities, proportions, combinations and varieties of different foods, drinks and nutrients, and the frequency with which they are consumed. DLPs refer to a combination of a certain dietary pattern with other measures such as body weight and behaviour-related risk factors including physical activity, alcohol consumption and smoking.
The insights presented in the report can support improvements in cancer prevention strategies, including policy guidance and help populations around the world to adopt healthy DLPs.
The work is part of WCRF International’s Global Cancer Update Programme – the world’s largest source of scientific research on the impact of diet, nutrition, physical activity, and body weight on cancer prevention and living with and beyond cancer.
Two research teams from the Harvard T.H. Chan School of Public Health and the Health Research Institute of the Balearic Islands used CUP Global methodology to conduct a comprehensive review of the research on colorectal and breast cancer incidence and mortality.
WCRF International worked with an expert panel who judged the evidence and made recommendations on the characteristics of a cancer-preventing DLP.
Global Cancer Update Programme collaborator and Professor of nutrition and epidemiology at the Harvard T.H. Chan School of Public Health, Prof Edward Giovannucci, said:
“The work by the Global Cancer Update Programme in reviewing and synthesising the literature on the role of dietary and lifestyle patterns in relation to colorectal cancer risk and mortality represents an immense step forward in how healthy lifestyle habits are key to prevention of cancer.
“The major advancement of this project is in the development of methods of synthesising the data on diet and lifestyle in a more holistic manner, rather than examining piecemeal specific components such as individual foods and nutrients.
“These new findings strongly support that adopting a healthy pattern of diet, maintaining a healthy weight, staying physically active, and embracing health-conscious habits, such as avoiding tobacco and moderating alcohol, are collectively associated with a lower risk of colorectal cancer.”
For colorectal cancer, the panel analysed 86 studies. Based on this evidence, they have recommended a DLP for reducing the risk of bowel cancer that includes:
- Maintaining a healthy weight and regularly taking part in physical activity
- Prioritising fruit and vegetables, as well as fibre-containing foods
- Consuming coffee and food and beverages that contain calcium such as dairy products
- Reducing the consumption of sugar sweetened beverages and alcohol
- Avoiding smoking
- Avoiding eating processed meats
For breast cancer incidence and mortality, the panel assessed 84 research publications and recommended a DLP that includes:
- Maintaining a healthy weight and regularly taking part in physical activity
- Prioritising fruit and vegetables and fibre-containing foods
- Lowering consumption of red and processed meat and sugar-sweetened beverages
- Avoiding alcohol and smoking
Global Cancer Update Programme collaborator and Lead Researcher at the Health Research Institute of the Balearic Islands and the Physiopathology of Obesity and Nutrition Networking Biomedical Research Centre, Dr Dora Romaguera, said:
“Globally, breast cancer is the most common cancer among women. We have conducted the first comprehensive synthesis of the totality of the evidence on the associations between dietary and lifestyle patterns and breast cancer risk.
“Our findings are strengthened by the robust approach to critically assessing the strength of the evidence as part of the Global Cancer Update Programme.
“This report provides clear evidence that by looking at our whole diet and the way we live, there are clear steps to recommend to women to lower their breast cancer risk. Importantly, this work highlights the greatest benefit is found when adhering to most aspects of a cancer preventative pattern simultaneously.
“By looking out our whole diet and the way we live, there are clear steps we can take to minimise our risk of breast cancer.”
In the report, the panel gave a range of recommendations on how to encourage populations around the world to adhere to healthy DLPs. These include:
- It is important that our recommendation for a cancer preventative dietary and lifestyle pattern is tailored to the region. This will only be adopted by individuals and communities and be sustainable if it is seen as culturally acceptable. Because of this, we made every effort to ensure that the constituents are not prescriptive but can be adapted to include foods available globally.
- When developing or updating food-based dietary guidelines, awareness of how the diet impacts, and is impacted by, our changing climate should be communicated.
- For further policy tools to promote our recommendations and our dietary and lifestyle pattern, please refer to WCRF International’s Policy Blueprint. This includes principles for design and implementation of policies, and how policies can be developed to address health inequalities.
World Cancer Research Fund’s Executive Director of Research and Policy Dr Giota Mitrou, said:
“This report outlines barriers and opportunities that exist, which could either prevent or help populations stick to a healthy dietary and lifestyle pattern. A cancer preventative Dietary and Lifestyle Pattern is paramount to sustaining healthy nations and and we hope will have wider benefits for the health of our planet.
“Our recommendations are applicable to all and should also be adapted to reflect specific cultural traditions and local contexts. Dietary and lifestyle changes are unlikely to be possible without wider societal policies that allow for better access to healthy foods and other health behaviours related to cancer prevention.”
Read the published papers
> Breast Cancer and Dietary and Lifestyle Patterns paper
> Colorectal cancer and dietary and lifestyle patterns paper

Sign up to hear more from us
Get the latest cancer prevention-related news and updates straight to your inbox
 We’ve come across many examples of human rights being used to advance cancer prevention at the McCabe Centre – whether through public interest litigation by civil society in south Asia to introduce smoke-free public places, or through incorporating non-communicable disease (NCD) prevention and healthy diets into regional human rights strategies and reporting to UN human rights bodies in the Pacific.
We’ve come across many examples of human rights being used to advance cancer prevention at the McCabe Centre – whether through public interest litigation by civil society in south Asia to introduce smoke-free public places, or through incorporating non-communicable disease (NCD) prevention and healthy diets into regional human rights strategies and reporting to UN human rights bodies in the Pacific.
We were therefore pleased to see World Cancer Research Fund International’s recently launched Policy Blueprint recognise the co-benefits of cancer prevention and the fulfilment of human rights.
This blog aims to explain what these co-benefits are, and how those working in cancer prevention can make the most of them.
Cancer prevention is part of our human rights
The International Covenant on Economic, Social and Cultural Rights establishes that people have a right, and countries have a duty, to prevention, treatment and control of disease as part of the right to health. The Committee on Economic, Social and Cultural Rights, which is established under the Covenant to assist in its interpretation, outlines that in order to protect, promote and fulfil the right to health, countries need to regulate health-harming products and make preventive health services and health information available, accessible, acceptable and good quality. The UN Special Rapporteur on the Right to Health, an independent expert on human rights whose mandate is established under the UN Human Rights Council, has endorsed a number of cancer prevention measures as a means of fulfilling this right, most specifically in relation to front-of-pack food labelling and promoting and supporting breastfeeding.
Likewise, the Committee on the Rights of the Child states that children’s right to health in the Convention on the Rights of the Child includes government obligations to address childhood obesity. This includes limiting children’s exposure to fast foods that are high in fat, sugar and salt or energy dense and nutrient poor, and regulating their marketing and availability in schools and other public places.
Grounding prevention policies in human rights
In many countries, human rights law can provide a valuable framing for engagement with ministries outside of health. In Argentina, civil society organisations successfully advocated for front-of-pack food labelling in parliament using a campaign strongly grounded in human rights. This included emphasising consumers’ right to information on whether foods had levels of sugar, fat and sodium that would harm health, and the right to healthier food environments as a component of the rights to food and health.
In Norway, the WHO’s guideline on policies to protect children from the harmful impact of food marketing, which is aligned with obligations under the Convention on the Rights of the Child, has been important to the Ministry of Health’s recent announcement of its plans to ban the marketing of junk foods to children.
The Committee on the Rights of the Child has raised concerns about commercial marketing in digital environments, including the profiling of children’s personal data for targeted marketing and the use of manipulative advertising techniques. The Committee has made recommendations that have been incorporated into UNICEF/WHO tools to support Member States to address the marketing of unhealthy foods to children. These connections between the marketing of unhealthy foods to children and a broader range of problematic digital commercial practices provide an opportunity to connect cancer prevention challenges to broader issues of online privacy, digital surveillance, and the rights of children in online spaces, and build alliances on these issues.
Cancer places an unequal burden on already marginalised or under-served communities, who are also more exposed to many cancer risk factors. A human rights approach, with its emphasis on ensuring that no one is left behind, and community participation and accountability, is a way of making sure that we have an equitable response that respects, protects and fulfils the rights of each individual to health. In her report on food, nutrition, and the right to health, the UN Special Rapporteur, Tlaleng Mofokeng, describes how disadvantaged groups are targeted in food marketing, and calls for more attention to be given to the relationship between NCDs, racial discrimination and gender.
Challenging the co-option of human rights by unhealthy industries
Despite human rights bodies’ recommendations to prevent cancer and regulate third parties’ impact on health, commercial interests such as the tobacco, alcohol or food industries are often more adept and better resourced at using this body of law than cancer prevention advocates. Unhealthy industries often invoke rights in litigation against public health laws, as part of a trend to launch legal challenges under trade, investment and constitutional law as a means of blocking public health policy. In Mexico, food companies launched a constitutional challenge to front-of-pack food labelling, arguing that it discriminated against food companies and restricted their right to trade.
Courts consistently reject these arguments, recognising that the rights of commercial actors must be balanced against other societal interests, including the rights of people to health, and that it does not enhance rights if we leave the marketing of harmful products by powerful commercial entities unchecked. The Supreme Court of Mexico upheld the front-of-pack labelling law, finding that the labels furthered the right to health and did not present a barrier to commerce. These challenges demonstrate the importance of proactively engaging with human rights and the law as part of a broader strategy on cancer prevention, so that lawyers representing commercial entities are less able to co-opt human rights to block public health policy.
A need for strategic alliances
Human rights are ultimately allies in implementing evidence-based laws to fulfil people’s right to health, with legal principles that emphasise equity, the right of consumers to be informed, and government obligations to regulate commercial actors that may harm human rights all fitting in well with public health objectives. Recalling these principles and building strategic alliances with human rights groups means we can better realise the potential of cancer prevention policies to promote and fulfil human rights for all.
The author would like to acknowledge Hayley Jones and Clare Slattery for comments on an earlier draft of this article.

Get the latest policy news first
Sign up to receive our monthly digest of nutrition and physical activity-related policy developments
In almost every region of the world, overweight and obesity among children and adolescents is a public health problem. There has been no progress in stemming the rate of overweight and obesity in children under 5 years in nearly 20 years, according to the World Health Organization (WHO).
This is a problem, because we know that when people live with overweight or obesity near the start of their lives, it often becomes a challenge throughout their adult lives.
What’s the problem with being inactive?
Young people may not be thinking very much about their risk of developing cancer. But the habits laid down in youth can last a lifetime. Our evidence shows that being active reduces the risk of colon (part of the bowel), post-menopausal breast and womb cancers.
Perhaps more importantly, being physically active also helps reduce our risk of living with overweight and obesity – a cause of at least 13 different types of cancer. Put simply, excess weight results from an imbalance between the energy we take in through our diet, and the energy we expend through being active (and other bodily functions). While we need to consider wider issues related to our ability to access a healthy diet, and managing stress and sleep levels, part of the solution involves being more active.
Are screens a particular problem?
Screens, and particularly mobile phones, have been blamed for a range of social and health problems among young people, including:
Evidence from our 2018 Diet and Cancer Report revealed convincing evidence that more screen time for children (from mobile phones but also using computers at school and watching devices during leisure time) makes weight gain more likely, as well as overweight and obesity.
The reasons for this are mixed. We tend to watch screens while sitting down, which uses less energy. Watching screens can also encourage us to eat more than is needed, not least because of exposure to adverts for unhealthy food and drinks, which young people may be particularly susceptible to.
The WHO lists limiting screen time as one of the ways to prevent and manage overweight and obesity in young people – but it’s only one.
What are the barriers to getting more active?

Young people’s experiences differ but, looking at the evidence and talking to parents and teenagers in the UK, a few common problems are highlighted:
- Underfunded / poor-quality equipment in public spaces (that may also feel unsafe to use).
- Cost – young people often don’t have a steady income, and gyms/clubs/sports can be expensive. Young people need access to parks and sports fields in their neighbourhoods.
- Travel – young people are often dependent on others for travel, which makes active travel – including safe routes to walk or cycle to school – and good public transport infrastructure so important (see below).
- Lack of options – children and young people in the UK are often offered activities such as football, netball and cross-country, but many want to try out less conventional sports such as yoga, dodgeball or trampolining.
- Gender – there is a significant decline in young girls taking part in sport, and parents of girls highlighted particular barriers to participation around body image, concerns about sweating and clothing, and lack of private changing spaces.
Elsewhere, a 2022 study looking at Botswana, Ethiopia, South Africa and Zimbabwe identified barriers around funding, but also highlighted community safety and a general lack of infrastructure as challenges.
What solutions are working around the world?
When developing ideas and designing policies to tackle overweight and obesity among children and young people, one voice is often unheard – that of young people themselves. From 2018–23, World Cancer Research Fund was involved in an innovative EU-funded project called CO-CREATE, which aimed to change that by putting young people at the forefront of tackling the obesity epidemic in Europe. The youth representatives on the project came up with 4 demands to policymakers, including “Offer all children and adolescents free, organized physical activities at least once every week.”
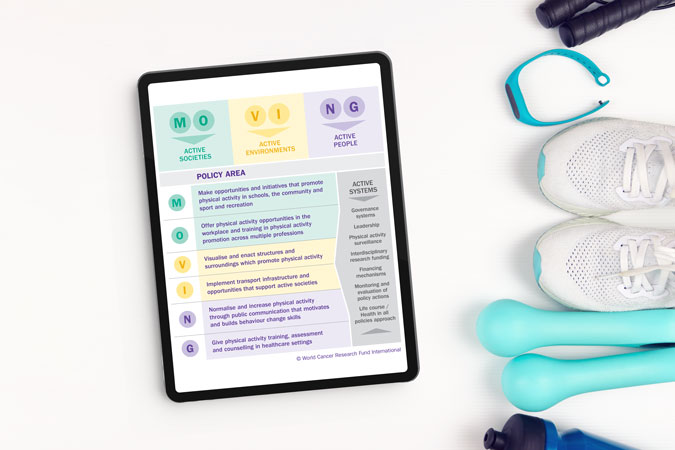
Using what they learned as part of the CO-CREATE project, our Policy team have devised a policy factsheet on physical activity, outlining the best ways to meet our Cancer Prevention Recommendation to be physically active.
Of all the information in the factsheet, some policy recommendations would specifically benefit children and young people, if acted on by governments around the world. These include:
- Initiatives that optimise opportunities for physical activity (including walking and cycling to and from school).
- Active play before and after school, as well as during recess and lunch breaks.
- Reduce sitting during classes.
- Policies to priorities active urban design, like ensuring access to open/green space or walking and cycling infrastructure where people live.
To keep people informed about both the need to be active, and the opportunities available to them, we also recommend:
- High quality physical education in school curricula.
- Enhanced physical activity training for all teachers.
And some of these innovative policies are already being undertaken in parts of the world. There are many policies recorded in our MOVING database mandating physical activity in schools, broadly ranging from 2–4 hours per week, depending on age and country.
And it’s not just dedicated PE sessions. Italy’s Scuola attiva kids aims to promote a culture of wellbeing and movement among not only students but teachers and families as well. In Finland, the Students on the Move programme encourages young people to sit less and move between breaks. Belgium’s Adventurous Activity initiative offers young people the chance to try out high and low ropes, tree climbing, rowing, BMX, skiing and orienteering.
Yet parents we spoke to suggested that there also needs to be a reframing of how PE is seen in school. One parent in Surrey, UK, said: “If you’re really good, you tend to do loads as part of a club, but there seems to be very little for those who aren’t any good.”
“There’s different aspects of sports. There’s one where you’re trying to create lifelong fitness for young people to engage in sport as part of a healthy lifestyle. And there’s another part where you need competitive sport to provide appropriate challenge” – Jennifer Cole, teacher and parent of 3, Brunei
“Emphasise fun so everyone can join in. Let people compete and win something but focus on beating personal bests rather than being top of the class so it’s not exclusive. Why not offer points or vouchers for those who increase their steps the most, not the ones with the overall highest numbers, so you’re encouraging people who don’t do anything?” – Mike, parent of 3 including 2 teenage girls, UK
Active travel was another key concern for parents – and is also one of our policy recommendations, including:
- Transport policies, systems and infrastructure that prioritise walking, cycling and use of public transport.
- Road safety actions for pedestrians and cyclists.
Active travel, which has the additional benefit of helping countries meet climate commitments, is already being promoted in many European countries. Austria’s Kindergarten Mobility Box aims to make walking and cycling the norm from a young age, and Belgium has similar scheme.
Perhaps, rather than just focusing on crisis-driven solutions to an increasingly inactive world, we need to listen more to young people about the changes they want to see in their world, alongside implementing policies that make it easier for everyone – especially young people – to move more and sit less as part of their everyday lives.
Want to get more active?
Check out our resources to help you get moving – written by experts