We’re excited to announce that World Cancer Research Fund has joined Our Future Health, the UK’s largest health research programme, as an affiliate partner.
With cancer rates rising and modifiable factors contributing to around 40% of all cases, the partnership represents a bold step in harnessing large-scale health data and decades of scientific insight to prevent more cancers before they start.
The UK Director at World Cancer Research Fund, Steven Greenberg, said:
“It’s tremendously exciting to be a part of the UK’s largest, most diverse health research programme. We know that 40% of cancers can be prevented through modifiable factors such as diet and exercise. With a growing rate of diagnoses, collaboration to better understand these risks is more important and timelier than ever.
“By working together, we’ll be able to combine our own extensive knowledge and experience on cancer prevention with the knowledge and insight coming from Our Future Health to further understand how cancer risk can be affected by diet and lifestyle.
As an affiliate partner, we’ll contribute our global expertise in the links between diet, weight, physical activity and cancer risk, helping guide Our Future Health’s work in identifying preventable risk factors. In turn, we’ll benefit from collaborating with the UK’s largest health research programme – enabling new insights into early detection and public health strategies.”
About Our Future Health
Our Future Health is the UK’s largest ever health research programme. It is designed to help people live healthier lives for longer through the discovery and testing of more effective approaches to prevention, earlier detection and treatment of diseases. Our Future Health is inviting millions of people, from all backgrounds and from across the UK, to take part. Volunteers are providing information about their health and lifestyles to create an incredibly detailed picture that represents the whole of the UK.
Dr Raghib Ali, CEO and Chief Medical Officer of Our Future Health, said:
“We’re so pleased to welcome World Cancer Research Fund as our newest affiliate charity partner. We know that cancer will affect half of us in our lifetimes, and together we want to improve cancer prevention, so more people can live longer, healthier lives. Their expertise in funding life-saving research will be really valuable for Our Future Health.”
As part of Cancer Prevention Action Week 2025, on Wednesday we handed in an open letter and petition, alongside breast cancer survivors Dr Liz O’Riordan and Nikki Bednall, and the Alcohol Health Alliance.
The letter (below) – signed by more than 25 organisations and health experts – and the petition called on Prime Minister Sir Keir Starmer and his government to introduce a National Alcohol Strategy to Prevent Cancer, as part of our Cancer Prevention Action Week (CPAW) activity.
This year, CPAW is highlighting the links between alcohol and cancer – our research shows that most people don’t know that drinking any amount of alcohol increases the risk of 7 types of cancer.
What’s more, around 17,000 new cases every year are down to alcohol – so we’re urging the UK government to introduce a long-overdue National Alcohol Strategy for England – one that tackles alcohol harm head-on through:
- mandatory health warnings highlighting cancer risk
- minimum unit pricing
- marketing restrictions
to reduce consumption, lower cancer risk, and protect lives.





Read the full letter below
The Rt Hon Keir Starmer MP
Prime Minister
10 Downing Street
London SW1A 2AA
CC: The Rt Hon Wes Streeting MP, Secretary of State for Health and Social Care
Ashley Dalton MP, Parliamentary Under-Secretary of State for Public Health and Prevention
25 June 2025
The UK government must act on alcohol now to prevent cancer
Dear Prime Minister,
On behalf of more than 20 organisations and public health leaders, we are writing to share our deep concern about the continued lack of action to reduce alcohol consumption across the United Kingdom. In particular, the absence of a National Alcohol Strategy for England stands in stark contrast to the scale of harm caused by alcohol, with alcohol-specific deaths having increased by 42% in England between 2019 and 2023 alone.
This week marks Cancer Prevention Action Week (CPAW) – a national campaign led by World Cancer Research Fund (WCRF) – which seeks to empower the public and inspire change to prevent cancer. This year, CPAW is shining a spotlight on the link between alcohol and cancer, and the urgent need for government action.
In the UK, alcohol causes around 17,000 cases of cancer every year – equivalent to 46 people receiving a diagnosis every single day. And as our population ages and grows, these numbers are projected to rise. Worryingly, the pandemic has also driven an increase in high-risk drinking. Modelling by the Institute of Alcohol Studies and Health Lumen suggests that if this trend persists, we could see an additional 18,785 cancer cases by 2035.
Public awareness remains alarmingly low that alcohol is a Group 1 carcinogen, the same category as tobacco and asbestos, and a cause of seven types of cancer, including two of the most common breast and bowel as well as mouth and throat, oesophageal, liver and stomach cancer. These risks are present even at low levels of consumption. New polling commissioned by WCRF reveals that when asked unprompted only 1 in 14 UK adults are aware that alcohol increases cancer risk and 25% believe there is no health risk attached to drinking alcohol.
We are not alone in our concern – thousands of members of the public including more than 20 organisations have signed our petition calling for greater government action. They agree that no one should have to suffer the devastating trauma of alcohol-related cancer.
The human toll is compounded by the economic burden. In 2016, Cancer Research UK estimated that alcohol-attributed cancers cost the NHS alone an estimated £100 million annually. With the health service under immense strain, it is imperative to act now and realise the government’s priority of prevention.
Despite alcohol being the sixth leading cause of preventable cancer in the UK, current policy does not reflect this reality. We urge the government to fulfil its responsibility to protect public health by introducing a National Alcohol Strategy for England without delay, which must include:
- Mandatory alcohol product labelling with health warnings, including information on cancer risks and calorie content.
- Marketing restrictions on alcohol by classifying it as an ‘unhealthy product’ under high fat, salt and sugar marketing restrictions.
- Implementing and evaluating minimum unit pricing at 65p in England with rates adjusted in line with inflation, to bring England into line with Scotland, Wales and Northern Ireland who all either have MUP already or have stated their intention to implement.
It is vital that this strategy aligns with the forthcoming National Cancer Plan for England, ensuring that alcohol is comprehensively addressed as a modifiable risk factor for cancer. We also urge the UK government to work in close collaboration with the devolved administrations, particularly to enable action to improve approaches to labelling and advertising. All policy development processes must be protected from industry influence and vested interests to ensure public health is placed above profit.
Such action would not only help to reduce cancer risks but reduce other alcohol-related harms. It would also support the government’s own ambitions to shift from sickness to prevention, as set out in the Health Mission, and contribute to economic growth by reducing illness-related inactivity.
We stand ready to support this effort and urge you to act now. Together we can tackle the devastating impact of both alcohol harm and cancer.
Yours sincerely,
Rachael Gormley, Chief Executive, World Cancer Research Fund
Dr Richard Piper, CEO, Alcohol Change UK
Alison Douglas, Chief Executive, Alcohol Focus Scotland
Professor Sir Ian Gilmore, Chair, Alcohol Health Alliance
Greg Fell, President, Association of Directors of Public Health
Dr Heather Grimbaldeston, Chair, BMA Public Health Medicine Committee, British Medical Association
Professor David Strain, Chair, BMA Board of Science, British Medical Association
Thalie Martini, Chief Executive Officer, Breast Cancer UK
Eddie Crouch, Chair, British Dental Association
Pamela Healy OBE, Chief Executive, British Liver Trust
Jill Clark, Chair, CancerWatch
Alison Wise, Communications Manager, on behalf of Fight Bladder Cancer
Ailsa Rutter OBE, Director, Fresh and Balance
Kostas Tsilidis, Associate Professor of Cancer Epidemiology and Prevention, Imperial College London
Dr Katherine Severi, Chief Executive, Institute of Alcohol Studies
Dr Dominique Florin, Medical Director, Medical Council on Alcohol
Daniela Binnington Nessman, Founder, Menopause and Cancer
Gopika Chandratheva, Nutritionist, NHS
Tamara Khan, CEO, Oracle Head & Neck Cancer UK
Jon Coleman-Reed, Head of Operations, Prevent Breast Cancer
Dr Claire Shannon, President, Royal College of Anaesthetists
Robert Steele, Chair, Board Directors, Scottish Cancer Foundation
Dr Alastair MacGilchrist, Chair, Scottish Health Action on Alcohol Problems
Chris Curtis, Chief Executive Officer, Swallows Head & Neck Cancer Support Charity
Amandine Garde, Professor of Law & Non-Communicable Diseases Research Unit, University of Liverpool
Richard Cooke, Professor of Health Psychology, University of Staffordshire
Dr Kathryn Scott, Chief Executive, Yorkshire Cancer Research
Only 16% of us in the UK feel at ease discussing our relationship with alcohol, ranking it among the least talked about topics – less so than sex (17%) and money (29%), according to our poll.
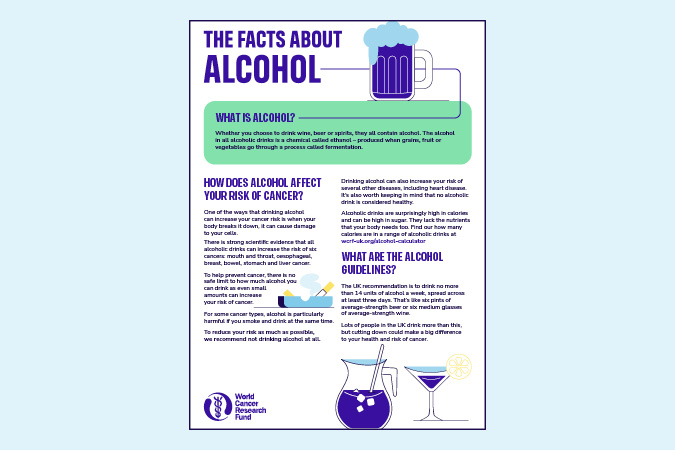
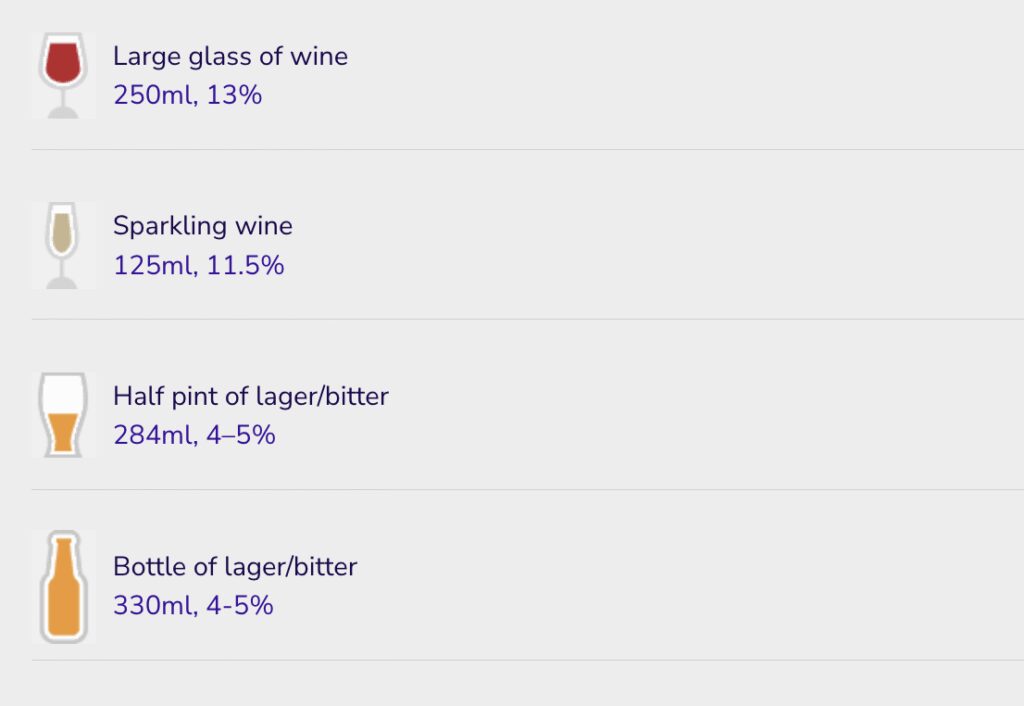
We’re emphasising the connection between alcohol and cancer as part of Cancer Prevention Action Week, which starts today. We have strong evidence that alcohol increases the risk of 7 cancers:
- Breast
- Bowel
- Head and neck
- Oesophageal
- Liver
- Stomach
Alcoholic drinks are also high in calories and often high in sugar, increasing the risk of gaining weight. Living with overweight or obesity increases the risk of at least 13 types of cancer.
We surveyed 2,000 people to gain insights into Britain’s understanding of alcohol and cancer risks. The findings reveal consistent misconceptions regarding alcohol’s dangers. Alarmingly, 25% of respondents did not associate any health risks with alcohol, and only 1 in 14 mentioned cancers as a risk when asked unprompted.
These misconceptions may hinder our ability to have informed conversations about alcohol. About 4% of cancer cases in the UK are attributed to alcohol, meaning that, each year, around 17,000 people are diagnosed with cancer caused by alcohol. Adding to this immeasurable human cost is the economic burden. Alcohol-related cancers cost the NHS around £100m every year.
We need a National Alcohol Strategy
We support clearer public health messaging to raise awareness of the real dangers of alcohol consumption, as well as other measures such as health warning labels. Alongside many other health organisations in the UK, we’re urging the Prime Minister, Sir Keir Starmer, to implement a National Alcohol Strategy for England.
World Cancer Research Fund CEO Rachael Gormley
Alcohol is pervasive in our lives, from celebrations to after-work drinks. But do we truly understand the risks involved? It’s essential that we engage in more discussions about alcohol and cancer, empowering individuals to make informed health choices.
Alcohol Health Alliance Chair Sir Ian Gilmore
One of the reasons public awareness is so low is that we're being kept in the dark about the true cost of drinking. People have the right to know the full picture so that they can make informed choices about what they consume.
World Cancer Research Fund Executive Director of Research and Policy Dr Giota Mitrou
A long-overdue National Alcohol Strategy in England would help the government tackle alcohol harm head on – reducing consumption, lowering cancer risk, and protecting lives.
Nikki Bednall is a World Cancer Research Fund Supporter and breast cancer survivor. She said: “I always thought drinking a few times a week was fine. I never knew it could raise my cancer risk. If I’d known earlier, I might have made different choices. Though hindsight is easy, my perspective has changed with the knowledge that came after my diagnosis.”
Drinking habits in the UK paint a concerning picture in comparison with other nations. Organisation for Economic Cooperation and Development (OECD) 2021 data showed that alcohol consumption in the UK was 10 litres per capita – 16% more than the OECD average of 8.6 litres.
Covid led to an increase in the number of high-risk drinks, with the heaviest drinkers increasing their consumption the most. These changes have persisted beyond the national lockdowns of 2020 and 2021, and subsequently there has been a year-on-year rise in alcohol-specific deaths, which reached an all-time high of 10,473 in 2023.
The research was conducted by Opinion Matters, among a sample of 2,000 nationally representative UK adults. The data was collected between 21.03.2025–24.03.2025.
Cancer Prevention Action Week (CPAW)
This year we’re highlighting the links between alcohol and cancer.
Alcohol and cancer: let’s talk – that was the theme of this year’s Cancer Prevention Action Week. For 7 days on 23–29 June, we talked to politicians, gave radio interviews and spoke to experts about alcohol and cancer. Plus, we shared news and views across our socials:
Facebook | LinkedIn | Instagram | Bluesky
How Cancer Prevention Action Week unfolded
Monday’s highlights
> Brits find it harder to talk about alcohol than sex or money
Yorkshire GP speaks out in support of CPAW:
Dr Nigel Wells, Medical Director and Executive Director Clinical & Care Professional Humber and North Yorkshire ICB and practising GP:
As a GP, I know people can be reluctant to talk about alcohol or share concerns about their drinking – so it doesn’t surprise me that only 2 in 10 people across Yorkshire and the Humber feel comfortable doing so.
But alcohol isn’t harmless – it increases the risk of 7 types of cancer, and, too often, people simply aren’t aware. If this campaign helps someone pause and ask whether alcohol might be affecting their health, and encourages them to speak to a healthcare professional, it will have made a real difference. We need to make these conversations as routine as those about smoking or diet – and that starts with creating a safe, non-judgemental space in every consultation.
We tabled an Early Day Motion in support of Cancer Prevention Action Week. And Alcohol Focus Scotland, a key supporter of this year’s campaign, tabled a motion in the Scottish Parliament on alcohol and cancer.
Tuesday’s highlights

Alcohol Focus Scotland organised a photo call at Holyrood with Members of the Scottish Parliament (MSPs). Photographed are 11 MSPs, including the Cabinet Secretary for Health Neil Gray; Jackie Baillie, Labour’s deputy leader and health spokesperson, and Presiding officer Alison Johnstone. Read more on LinkedIn
Sheridan Dixon, of South Tyneside, was interviewed on ITV Tyne Tees about how she has reduced her drinking as part of efforts to stay cancer free. We’re grateful to our partner Balance North East for helping us share Sheridan’s story.
Wednesday’s highlights

We headed to No 10 Downing St to present our petition to UK Prime Minister Sir Keir Starmer.
Prof Lord John Krebs, Chair of our Global Cancer Update Programme, tabled questions in the Lords on the links between alcohol and cancer, keeping the issue high on the political agenda:
Lord Krebs’ questions to the Lords
-
1
Lord Krebs to ask His Majesty’s Government what steps they are taking to reduce alcohol consumption as a modifiable risk factor for cancer.
-
2
Lord Krebs to ask His Majesty’s Government whether the national cancer plan for England will address alcohol consumption as a modifiable risk factor for cancer.
-
3
Lord Krebs to ask His Majesty’s Government what assessment they have made of public awareness levels of the link between alcohol consumption and cancer risk.
-
4
Lord Krebs to ask His Majesty’s Government what consideration they have given to classifying alcohol as an unhealthy product under high fat, sugar and salt marketing restrictions to (1) strengthen limits on alcohol advertising, and (2) reduce alcohol exposure among vulnerable populations, including children and adolescents.
-
5
Lord Krebs to ask His Majesty’s Government what assessment they have made of the impact of minimum unit pricing on alcohol-related cancer incidence.
CPAW supporter Prof Richard Cooke published research showing that policymakers and drinkers are speaking different languages when it comes to alcohol consumption. He says: “Policymakers need to construct policies to reflect the importance of emotions in drinkers’ narratives. This fits in with psychological theories of drinking behaviour which propose that people drink for different reasons.”
> The language of alcohol: Similarities and differences in how drinkers and policymakers frame alcohol consumption, published in Drug and Alcohol Review
Thursday’s highlights
Health professionals can be instrumental in helping individuals reset their relationship with alcohol and we supported them with a free webinar on Alcohol and cancer risk: What every health professional needs to know.
In the This Is Powerful podcast, Paul Sculfor talked to nutrition expert Dr Federica Amati about alcohol and cancer.
Friday’s highlights
On the blog: It’s mocktail Friday! Start your weekend early with some fizzy fruity creations
Saturday and Sunday’s highlights
Time to take a breath … alcohol is a major part of how many of us socialise, relax and celebrate. But nearly 4% of cancer cases in the UK are down to alcohol – around 17,000 new cases every year.
We hope this Cancer Prevention Action Week has given you an insight into the risks we’re all taking when we drink.
Our research shows that most people don’t know that drinking any amount of alcohol increases the risk of 7 types of cancer.
What happens next?
Cancer Prevention Action Week is just the start. We want to spark an ongoing national debate: with friends, family – and within government – about alcohol and cancer so that everyone can make more informed choices about their health.
But the UK government has said it won’t include mandatory comprehensive restrictions on alcohol marketing in its 10-year Health Plan – despite these being a proven, cost-effective way to reduce alcohol harm.
This is hugely disappointing. Contact the Prime Minister to make it clear that public health must be protected – and that cancer prevention cannot be sidelined.
On the blog
Media coverage
Cancer Prevention Action Week is across the news this week!
-
BBC Radio
Our Senior Policy Advisor, Kendra Chow, was invited to talk about this year’s campaign on BBC 5 Live on Saturday night. The interview was repeated across 5 Live and 43 other BBC radio stations.
-
Channel 5
Vanessa Feltz’s lunchtime show covered alcohol health warnings in a lengthy discussion including an interview with our supporter Dr Philippa Kaye.
Also on Channel 5, Jeremy Vine’s show discussed Alcohol labels should warn of cancer risk, urge health groups (The Times) in a round-up of the morning papers.
-
The Guardian
-
The Independent
-
The Times
-
The Telegraph
-
Julia Bradbury on Instagram
-
Scotland
-
International
- Mirage News (Australia)
- The Times of India
- Yahoo New Zealand
-
Science press
-
Trade press
-
Local press
- Rayo (Coventry and Nuneaton)
- This Is Wiltshire
- The Gazette and Herald
- Swindon Advertiser
- The Birmingham Mail
Facts at your fingertips
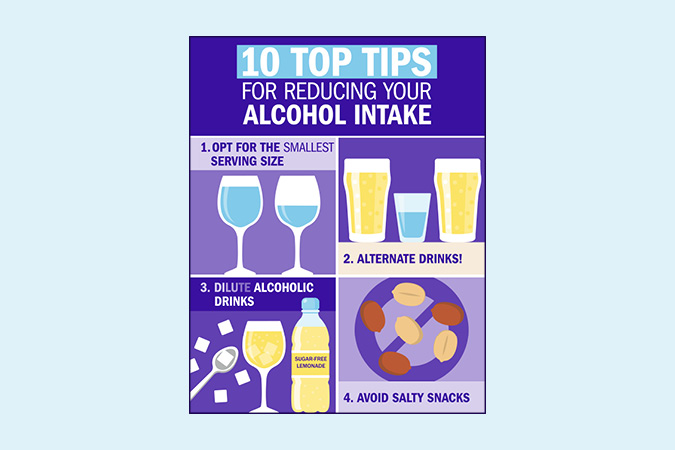
Written by experts, based on the evidence: our health resources unmuddle the myths about alcohol and cancer.
World Cancer Research Fund has responded to the UK government’s first multi-year spending review, where the Chancellor, Rachel Reeves, set out departmental budgets over the next 3 years.
Under their Health Mission, the government has committed to shifting from sickness to prevention, affirming that prevention is better than cure. This spending review marks a critical opportunity for the government to set out their investment to this commitment.
In this review, the Chancellor committed:
- £29bn for the day-to-day spending of the NHS to 2028–29.
- £80m per year for tobacco cessation programmes and to support the delivery of the Tobacco & Vapes Bill.
- £10bn in NHS technology and digital transformation by 2028–29.
- £22.6bn per year for research and development by 2029–30, including medical research.
Responding to the spending review, World Cancer Research Fund’s Executive Director of Research and Policy, Dr Giota Mitrou, said:
Today the Chancellor reaffirmed Labour’s Health Mission, including their commitment to shift from treatment to prevention. 40% of all cancer cases are preventable: as leading experts in cancer prevention, we know that primary prevention remains the most sustainable and cost-effective way to tackle cancer and other non-communicable diseases.
For example, while we are glad to see that the government will be investing £80m per year to tackle tobacco, we need to see similar efforts applied to obesity and alcohol. The expansion of free school meals is a step in the right direction and the type of action we hope to see in the upcoming 10-year Health Plan.”
Research funded by World Cancer Research Fund has shown that people living with cancer who closely follow a sustainable and nutritious diet – the EAT-Lancet reference diet – have a lower risk of dying from cancer and from all causes.
This is the first study to look at the impact of the EAT-Lancet diet on people living with or beyond cancer – as opposed to the general population. Prof Sabine Rohrmann and her team at the University of Zurich, in collaboration with colleagues from another Swiss university, the UK and Austria, used UK Biobank data to see if closely following this diet – with its emphasis on eating a rich variety of plant foods – affected the risk of death for people with a cancer diagnosis at the time they were recruited for the study.
Studying more than 25,000 people with an average age of 60 years at recruitment, the researchers used dietary information collected in the UK Biobank to develop a score that reflected how closely participants followed the EAT-Lancet diet.
More support needed for people facing cancer
Of the 25,348 cancer survivors in the group studied, 4,781 people died during the study follow-up. Prof Rohrmann’s results showed modest links between closely following the diet and a lower risk of dying from cancer, and of dying from all causes. The researchers didn’t observe a link between the diet and dying from heart disease.
Almost 64% of the participants were female, and participants who followed the EAT-Lancet diet more closely were more likely to be female. However, this study confirmed previous evidence showing that people living with and beyond cancer do not tend to follow healthy diets after their diagnosis. This emphasises the need to help people form healthier habits and overcome the barriers to eating well, such as treatment side-effects affecting appetite and taste.
These findings highlight the importance of greater nutrition support and guidance for people facing cancer. Guidelines aimed at the general population are unlikely to consider the needs of people living with and beyond cancer. With a lack of evidence-based recommendations for this population, the gap can sometimes be filled by practices not supported by the science – such as excessive use of dietary supplements.
This evidence showing the benefits of the EAT-Lancet diet follows recent research by our Global Cancer Update Programme, which provided guidance for people with a breast or a bowel cancer diagnosis.
Prof Sabine Rohrmann
We specifically put the focus of our study on cancer survivors because we believe that it is important to encourage them to follow a healthy lifestyle. For this, we need more evidence and so far, research on lifestyle changes in cancer survivors is still scarce.
Dr Julia Panina, Head of Research Funding
This study provides important new evidence that following the EAT-Lancet reference diet may reduce the risk of mortality in people living with and beyond cancer. The focus on the consumption of plant-based foods reflects our Cancer Prevention Recommendations to eat more wholegrains, vegetables, fruit and beans, and to limit red and processed meat. Importantly, these findings also show that diets supporting cancer survivorship can promote more sustainable eating and help protect the environment.
The EAT-Lancet reference diet was created by a team of scientists (The EAT-Lancet Commission on Food, Planet, Health) in 2019. It is a mainly plant-based diet that, according to the Commission, addresses the environmental impact of food production and consumption better than most national dietary guidelines.
> Read the paper: Higher adherence to the EAT-Lancet reference diet is inversely associated with mortality in a UK population of cancer survivors
> On the blog: Plant-based diets: eating for our health and the planet
Researchers funded by World Cancer Research Fund have discovered that brisk walking is linked to a lower risk of 5 cancers:
- anal
- liver (hepatocellular carcinoma)
- small intestine
- thyroid
- lung
Using information stored in the UK Biobank – a large database of many different aspects of health – scientists explored the link between walking pace – slow, steady or brisk – and the risk of developing 28 types of cancer.
They confirmed that the link between brisk walking and a reduced risk of developing the 5 cancers was true, even after accounting for overall physical activity and total walking time.
Speeding up your walk could represent an easy, low-cost public health intervention to decrease cancer risk.
The paper, published in BMC Cancer, says:
“Adopting a brisk walking pace may represent a pragmatic target for public health interventions to decrease cancer risk, particularly in circumstances where increases in walking volume or frequency prove impractical.”
PhD student Michael Stein’s research was supported by funding from Prof Michael Leitzmann’s grant. This research was funded by World Cancer Research Fund as part of the WCRF International Regular Grant Programme.
> Read the full paper: Usual walking Pace and risk of 28 cancers– results from the UK biobank
Seed oils are made by extracting oil from the seeds of various plants, such as:
- Sunflower
- Rapeseed (also known as canola oil)
- Sesame
- Grape
- Flax
- Soybean
- Safflower
These oils are versatile and many are budget-friendly choices in the kitchen. Most have a neutral flavour and a high smoke point, which means they can handle high cooking temperatures – like when you’re frying or roasting – without breaking down or producing unpleasant flavours or potentially harmful compounds. This makes them a safer and more reliable option for everyday cooking.
A particular benefit of seed oils is that they are high in unsaturated fat – the type we should eat more of – and low in saturated fat, which we should eat less of. This makes them a healthier alternative to animal fats like butter and ghee.
Importantly, seed oils provide essential omega-6 fats, which our bodies can’t make so we need them from our diet. These fats support healthy skin, and help build and maintain our cells.
Seed oils and inflammation

You may have seen claims that seed oils cause inflammation. This is mainly because they contain an omega-6 fat called linoleic acid, which can be converted in small amounts into another fat called arachidonic acid – a compound involved in the body’s inflammatory response.
Some people worry that eating too much omega-6 could compete with omega-3 fats, which support heart and brain health, and have anti-inflammatory properties. The concern is that both fats share some pathways in the body, so too much omega-6 may reduce the impact of omega-3s and promote inflammation.
But research doesn’t support this idea. In fact, studies show that people who eat more linoleic acid – the type found in seed oils – often have lower levels of inflammatory markers in the body. Instead of cutting back on omega-6, it’s more important to focus on getting enough omega-3s in your diet by eating oily fish (like salmon), green leafy vegetables (like brussels sprouts) and nuts (like walnuts).
What about cancer risk?
When it comes to cancer, there’s no strong evidence to show that seed oils increase risk. What matters most is your overall diet – we recommend you eat a diet rich in fruit, vegetables, wholegrains, pulses, nuts, seeds and lean proteins like fish and chicken to support your long-term health and reduce cancer risk.
Seed oils in processed foods
Seed oils can be found in ultra-processed products like:
- shop-bought salad dressings
- mayonnaise
- cakes
- biscuits
- crisps
- sweet and savoury pastries
These foods are typically high in salt and sugar, and low in fibre, vitamins and minerals – not ideal for our health.
In fast food restaurants, oils may be reheated multiple times at very high temperatures, which can produce potentially harmful compounds. Most of us don’t cook like that at home.
But it’s important to remember – seed oils themselves aren’t the problem. The real issue is the overall quality of the processed foods that contain them. It’s these foods that are linked to a higher risk of obesity, heart disease, type 2 diabetes and some cancers.
That’s why one of our Cancer Prevention Recommendations is to limit fast food and processed foods that are high in saturated fat, salt and sugar.
So, should I avoid seed oils?
Not at all – and there’s no need to fear them. Seed oils can be part of a healthy, balanced diet. They’re low in saturated fat, provide essential omega-6 fats and offer useful nutrients like vitamins E and K, which support immune health and normal blood clotting.
As with all fats, it’s about using them wisely. They’re high in calories, so stick to small amounts – a teaspoon or a light spray is often all you need. Seed oils are versatile in the kitchen, perfect for roasting, stir-fries, baking, homemade salad dressings or as a healthier alternative to butter or ghee.
References
-
List of journals consulted
Johnson GH, Fritsche K. Effect of dietary linoleic acid on markers of inflammation in healthy persons: a systematic review of randomized controlled trials. Journal of the Academy of Nutrition and Dietetics [Internet]. 2012 Jun 21;112(7):1029-1041.e15.
Laurindo LF, Laurindo LF, Rodrigues VD, Da Silva Camarinha Oliveira J, Boaro BL, Araújo AC, et al. Evaluating the effects of seed oils on lipid profile, inflammatory and oxidative markers, and glycemic control of diabetic and dyslipidemic patients: a systematic review of clinical studies. Frontiers in Nutrition [Internet]. 2025 Feb 7;12.
Petersen KS, Maki KC, Calder PC, Belury MA, Messina M, Kirkpatrick CF, et al. Perspective on the health effects of unsaturated fatty acids and commonly consumed plant oils high in unsaturated fat. British Journal of Nutrition [Internet]. 2024 Oct 28;132(8):1039–50.
Pischon T, Hankinson SE, Hotamisligil GS, Rifai N, Willett WC, Rimm EB. Habitual Dietary Intake of n-3 and n-6 Fatty Acids in Relation to Inflammatory Markers Among US Men and Women. Circulation [Internet]. 2003 Jun 24;108(2):155–60.
Rett BS, Whelan J. Increasing dietary linoleic acid does not increase tissue arachidonic acid content in adults consuming Western-type diets: a systematic review. Nutrition & Metabolism [Internet]. 2011 Jan 1;8(1):36.
Su H, Liu R, Chang M, Huang J, Wang X. Dietary linoleic acid intake and blood inflammatory markers: a systematic review and meta-analysis of randomized controlled trials. Food & Function [Internet]. 2017 Jan 1;8(9):3091–103.
Siobhan McGeown
Siobhan was inspired to run by her parents (in main picture), who have both had cancer. She says: “After watching both my parents suffer from cancer (ovarian and prostate), as well as several other close family members, I want nothing more than to see better outcomes for cancer diagnoses, as well as better detection and testing before it gets to that stage.”
Angela Brooks (left, wearing cap)
 Angela was diagnosed with breast cancer in 2021 aged only 33. She’s currently in remission but still living with the impact of cancer, including early menopause. Angela told us about her training schedule: “Every 3 weeks, between rounds of chemotherapy, I set myself the goal of completing a 10k run.”
Angela was diagnosed with breast cancer in 2021 aged only 33. She’s currently in remission but still living with the impact of cancer, including early menopause. Angela told us about her training schedule: “Every 3 weeks, between rounds of chemotherapy, I set myself the goal of completing a 10k run.”
Sam Burton
 Sam says: “The decision to run for World Cancer Research Fund is driven by my Father’s recent diagnosis with kidney cancer, an event that has reshaped my perspective on life and illuminated the critical importance of cancer research and advocacy.”
Sam says: “The decision to run for World Cancer Research Fund is driven by my Father’s recent diagnosis with kidney cancer, an event that has reshaped my perspective on life and illuminated the critical importance of cancer research and advocacy.”

Jack Gibbons and family
Jack Gibbons
 This is Jack’s second marathon for us, having also run in 2018. He’s running in memory of his mum, Maggie, who received a diagnosis of very aggressive stage IV melanoma in late 2023 and passed away in January 2024.
This is Jack’s second marathon for us, having also run in 2018. He’s running in memory of his mum, Maggie, who received a diagnosis of very aggressive stage IV melanoma in late 2023 and passed away in January 2024.
Maggie was there to support Jack when he ran his first marathon and was there at the finish line of the London Landmarks half in 2023 to see him over the line. Her support meant the world to Jack and he’s proud to be able to run for her in 2025 and raise money for World Cancer Research Fund.
David Herlihy
 David sadly lost his Dad to cancer in April 2024, and his Mum has been diagnosed with cancer for the second time in 5 years. He’s dedicated to health and fitness, and has completed 5 marathons, an ironman and 2 ultra marathons.
David sadly lost his Dad to cancer in April 2024, and his Mum has been diagnosed with cancer for the second time in 5 years. He’s dedicated to health and fitness, and has completed 5 marathons, an ironman and 2 ultra marathons.
Hannah Stedman
 Hannah is running in memory of her amazing Mum, who “had a very quick battle with lung cancer in October 2023. She was diagnosed on the 3rd and had passed by the 24th. To say this experience was the hardest thing of my life is an understatement.”
Hannah is running in memory of her amazing Mum, who “had a very quick battle with lung cancer in October 2023. She was diagnosed on the 3rd and had passed by the 24th. To say this experience was the hardest thing of my life is an understatement.”
George White
 George is a mortgage broker based in the West Midlands and is motivated to run for us after recently losing his Godfather to cancer.
George is a mortgage broker based in the West Midlands and is motivated to run for us after recently losing his Godfather to cancer.
Eating a wide variety of food may reduce the risk of gastrointestinal cancers, according to research funded by the World Cancer Research Fund network* and published in the European Journal of Cancer.
Little is known about how eating a wide variety of food species, also known as food biodiversity, may benefit our health or affect our cancer risk. Food species refer to a distinct type of plant or animal, such as wheat, chicken, or salmon. For example, salmon, mackerel, and tuna are all separate food species, even though they share some biological traits and belong to the same food group. Similarly, rocket, lettuce and spinach count as separate food species, even though they are all leafy green vegetables. However, chicken and a chicken’s egg belong to the same food species even though they are different types of food.
This study is the first to examine how the number of different food types consumed, measured as Dietary Species Richness (the number of species an individual consumes per year) affects the risk of the following gastrointestinal cancers:
- Oesophagus
- Throat
- Stomach
- Bowel
- Colon
- Rectum
- Gallbladder
- Pancreas
- Liver
The study followed 450,111 cancer-free adults in 9 European countries from the European Prospective Investigation into Cancer and Nutrition cohort for 14 years. The researchers, from the International Agency for Research on Cancer, found that individuals with the most diverse diets, by including more food species in their diet, had a 23% lower risk of developing gastrointestinal cancers compared with those with the least variety. The risk decreased by 6% for every 10 extra species per year added to their diet. People can do this by including more variety in the types of fruit and vegetables they eat, for example, choosing to eat local and seasonal fruit and vegetables of different colours.
Food biodiversity includes eating different types of food that provide the necessary nutrients for maintaining health. Investigating food biodiversity is important because it has the potential to benefit public health and sustainable food systems.
Dr Helen Croker, our Assistant Director of Research and Policy, said: “Diets have become more limited in the types of foods eaten and they are often high in fat, sugar and salt. However, for cancer prevention, it’s important to eat a healthy, balanced and varied diet with plenty of wholegrains, pulses, vegetables and fruit.”
Dr Helen Croker
This study is particularly interesting because it looks at the number of different foods people eat and the impact it can have on their cancer risk, in particular gastrointestinal cancers. More research is now needed to confirm these findings and further explore the link between dietary diversity and cancer prevention.
Dr Inge Huybrechts
This study shows how a more diverse diet, including a large variety of species, could lower the risk of gastrointestinal cancers, emphasising the importance of eating a wide variety of foods. The idea behind a diverse diet consisting of many types of plants and animals species may provide essential nutrients for the body while also strengthening ecosystems, making them more resilient, productive, and sustainable.
This study was funded by Wereld Kanker Onderzoek Fonds based in the Netherlands, as part of the World Cancer Research Fund International network.
Another study from this grant looked at how food biodiversity is measured. Methods such as Hill numbers estimate the number of species, but it wasn’t clear whether these numbers could be compared across different study settings.
The findings showed that Dietary Species Richness is the most feasible way to measure and evaluate food biodiversity across various contexts, and considering high-, middle- and low-income countries. Regardless of which Hill number was used, however, all measures indicated that greater food biodiversity was associated with better micronutrient sufficiency and with lower rates of all-cause mortality, this latter association yet being strongest for Dietary Species Richness.
Achieving a balanced combination of exercise and controlling our waistline is far more effective in reducing our risk of cancer than doing just one or the other, according to a study funded by World Cancer Research Fund.
In the world’s first study looking at the effectiveness of combining these measures, we found that only doing one is not enough to lower our risk of cancer. The study, which looked at more than 300,000 people, found that:
- People not meeting World Health Organization (WHO) guidelines on waist circumference are at 11% greater risk, even if they are physically active.
- People not meeting WHO guidelines for physical exercise are at 4% greater risk, even if “abdominally lean” (ie they have a smaller waist).
- Achieving neither means a 15% greater risk.
The study – WHO guidelines on waist circumference and physical activity and their joint association with cancer risk (Lead researcher: Prof Michael Leitzmann, University of Regensburg) – was published in the British Journal of Sports Medicine.
Prof Michael Leitzman
We're excited about the insights we’ve uncovered regarding the interplay between waist circumference and physical activity in reducing cancer risk. Our findings highlight the value of addressing multiple factors together, showing that both maintaining a recommended waist size and being physically active are critical for cancer prevention. This research reinforces the importance of practical, achievable changes that can have a meaningful impact on health over time.
Dr Helen Croker
This is the first study to examine the independent and combined impact of waist circumference and physical activity levels. The findings underscore the importance of a holistic approach instead of focusing on a single factor to reduce cancer risk. Maintaining a healthy weight and, in particular, having a waist circumference within the recommended level and being physically active, along with eating a healthy diet, are all crucial steps to reduce cancer risk. People can start by making small, sustainable changes like incorporating regular movement into daily routines or choosing healthier food options.
World Cancer Research Fund has been at the forefront of cancer prevention in the UK and globally for decades. We developed Activ8, a free 8-week programme to encourage people to move more, eat well and reduce their cancer risk. Every step is backed by science and brings our Cancer Prevention Recommendations to life.